Introduction
|
Definition: Paget disease of the breast arises when mammary carcinoma cells involve the epidermis of the nipple. From that location, they may extend into the epidermis of the areola, the remainder of the breast, and even the chest wall.
Clinical Significance: The carcinoma cells within the epidermis typically cause itching or pain and gives rise to scaling, crusting, or bleeding.
Gross Findings: The nipple may appear inflamed and the skin may appear erythematous or ulcerated.
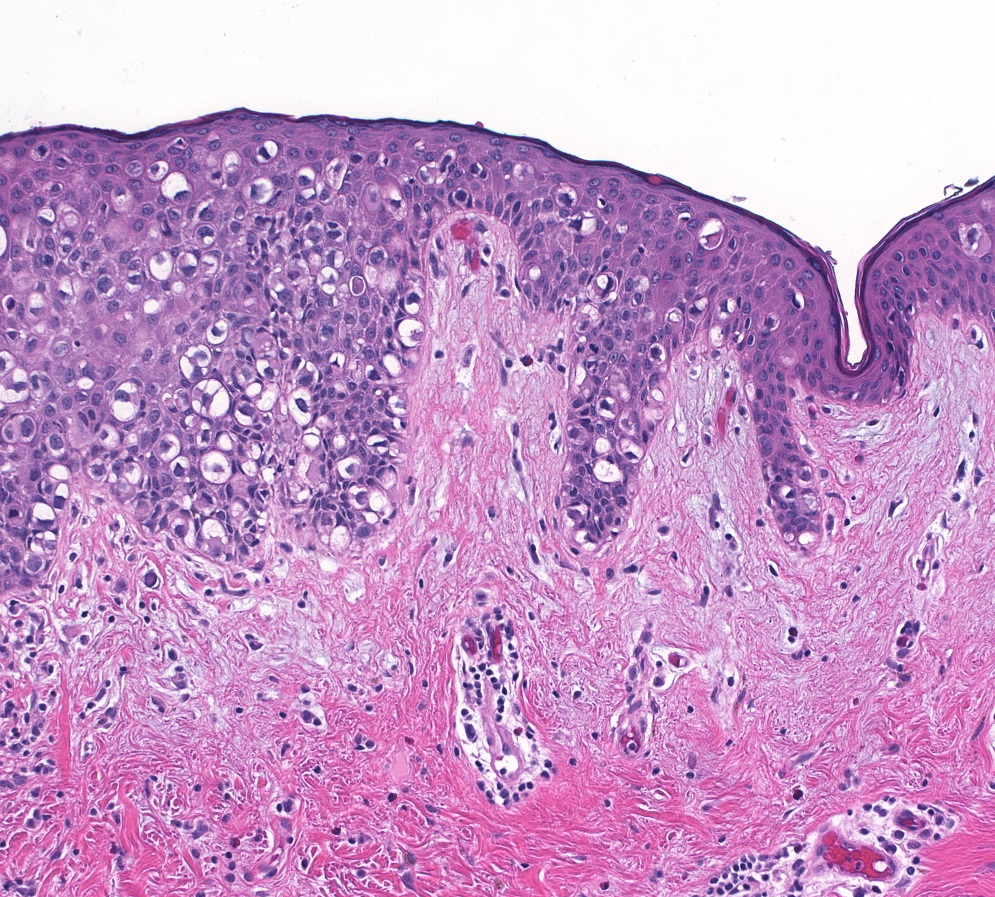
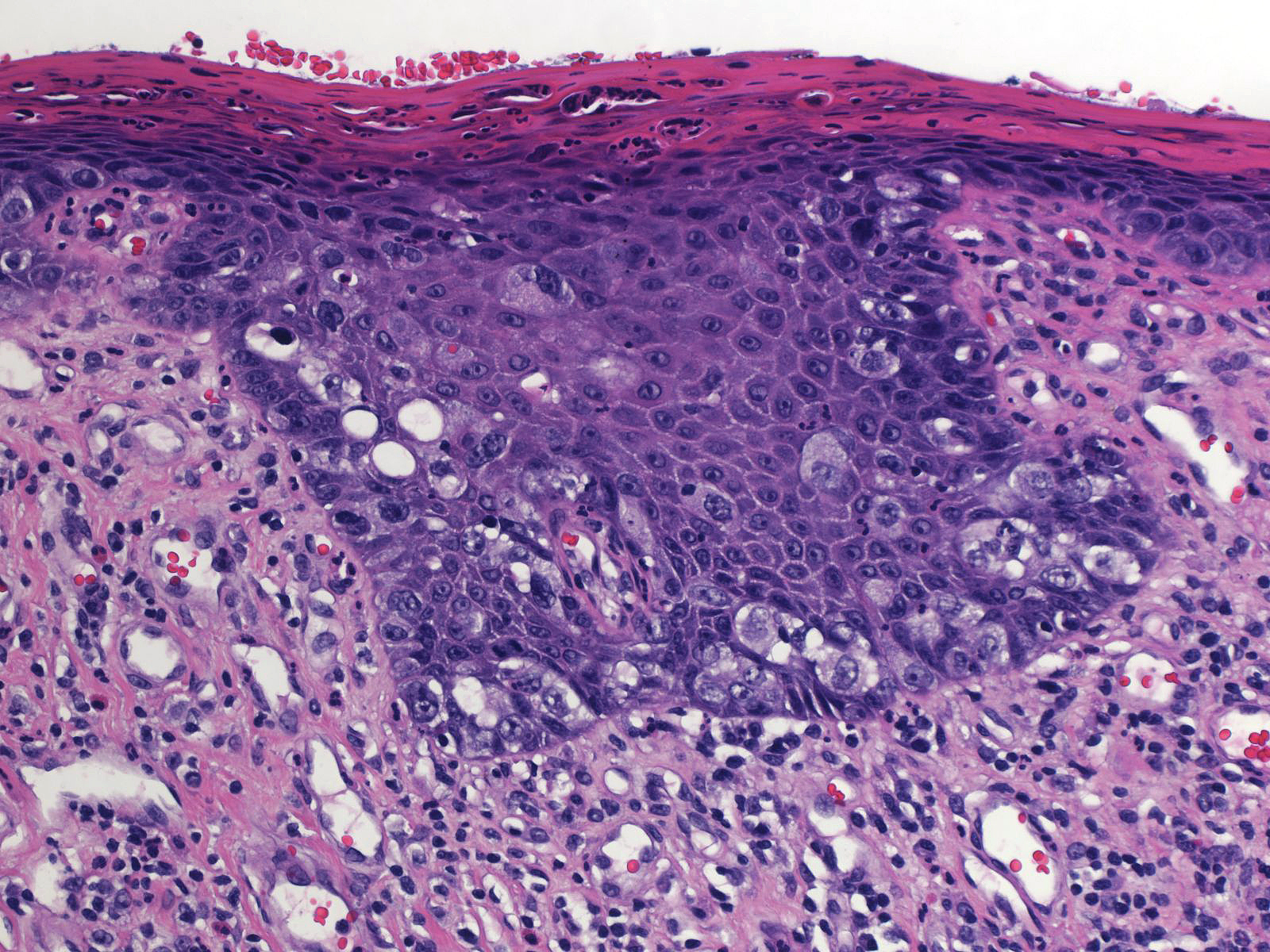
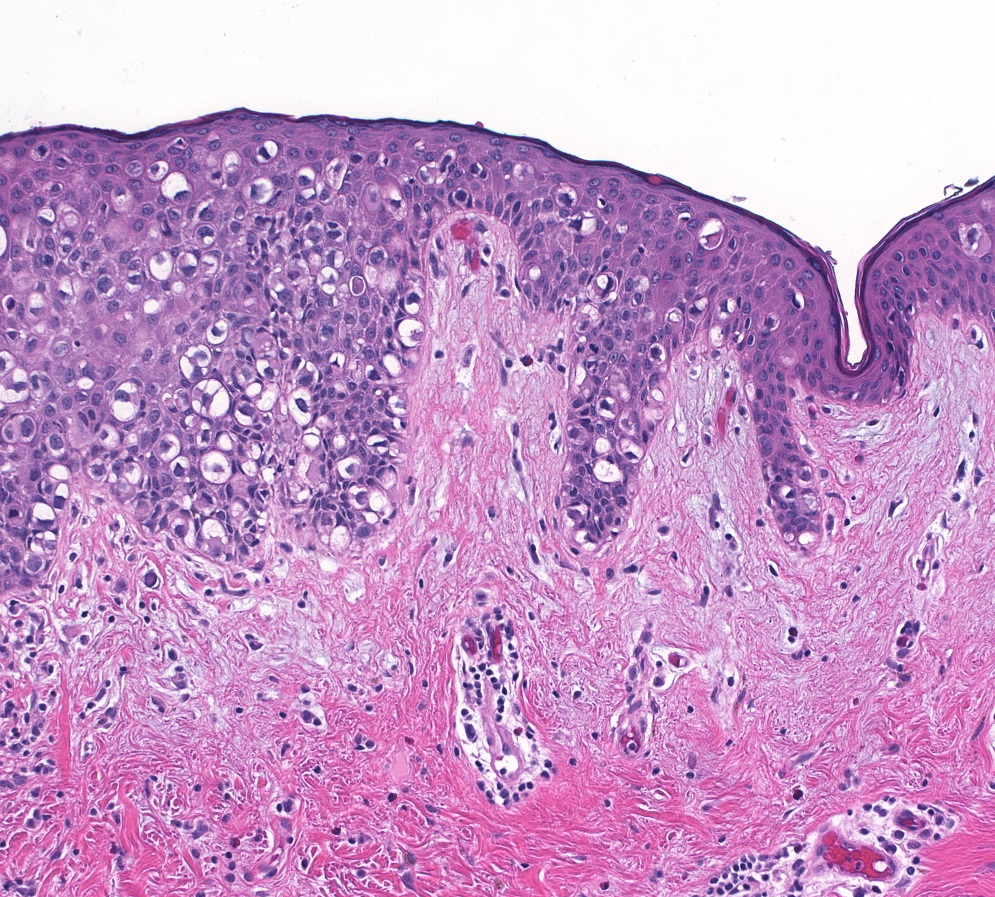
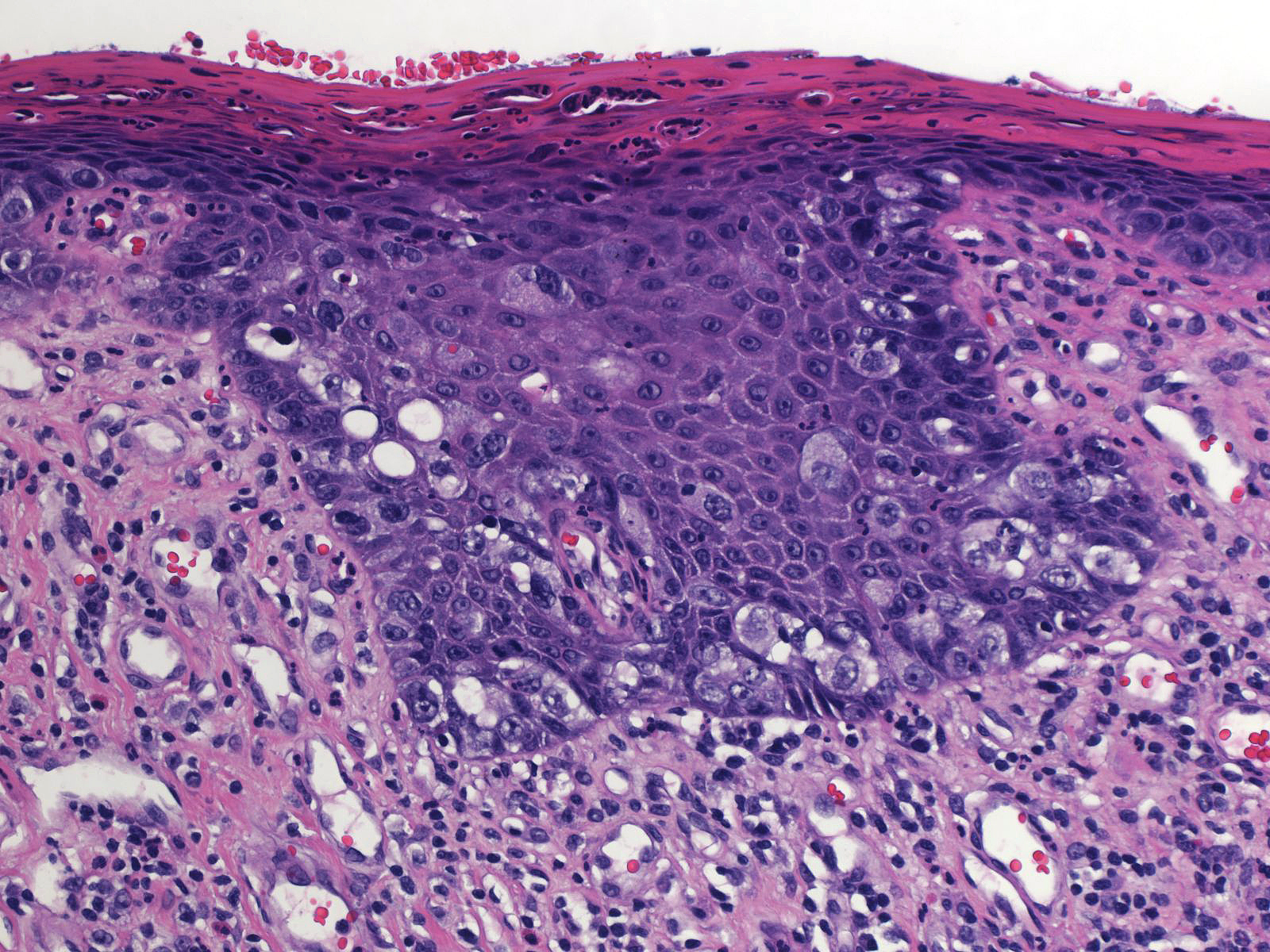
Microscopic Findings: Carcinoma cells percolate among the keratinocytes.
Differential Diagnosis: Glycogenated keratinocytes (mid-dermal location), Toker cells (lack of atypia), melanoma (melanocytic differentiation), squamous carcinoma (squamous differentiation)
Discussion: The carcinoma cells of Paget disease exhibit the cytological features of conventional high-grade ductal carcinoma. Special types of ductal carcinoma and lobular carcinoma do not ordinarily give rise to the clinical changes of Paget disease.
|
 In Paget disease of the breast, ductal carcinoma cells spread from the mammary ducts to the epidermis without penetrating the basement membrane. In Paget disease of the breast, ductal carcinoma cells spread from the mammary ducts to the epidermis without penetrating the basement membrane. |
| Paget cells appear large, and they possess large pleomorphic nuclei and easily seen nucleoli. The cells contain eosinophilic cytoplasm, which often contains mucin droplets. |
 |
|
|
| The chromatin varies from pale to dark. Dark chromatin may obscure the nucleoli. |
 |
|
|
| Although the malignant cells often grow in the basal region, they also usually extend into the superficial layers of the epidermis. |
 |
|
|
| An immunostains for cytokeratin 7 will highlight the carcinoma cells. Paget cells usually show intense (3+) staining for HER2 and overexpression of the HER2 gene. |
 |
|
|
| The involved epidermis and underlying dermis usually show reactive changes such as parakeratosis, hyperkeratosis, ulceration, and acute and chronic inflammation. |
 |
|
|
| The carcinoma cells can penetrate the epidermal basement membrane and invade the superficial dermis. |
 |
|
|
| In some cases of Paget disease, the clinical findings are extensive and striking. |
 |
|
|
Paget cells almost always contain engulfed melanin. It usually requires especially close examination to detect it; however, in uncommon cases, known as pigmented Paget disease, the carcinoma cells harbor so much melanin that they look like melanocytes and the lesion resembles a melanoma on clinical examination.
| Paget disease usually co-exists with an underlying high-grade ductal carcinoma. The co-existing carcinoma usually involves the nipple as well as regions of the gland distant from the nipple. The malignant cells in the skin and the co-existent carcinoma often exhibit similar cytological features, but may not appear identical. Genetic studies have revealed cytogenetic differences between the two populations in about half of cases. Uncommonly, carcinoma resides only in the nipple, and in rare cases it involves only the skin of the nipple. (Co-exisiting DCIS involving a large duct near the nipple) |
 |
|
|
| The differential diagnosis for Paget disease includes Toker cell hyperplasia. Toker cells lack significant cytoligic atypia and are usually few in number, but in occasional cases they can appear so numerous that it requires careful consideration to exclude Paget disease. In addition to lacking cytologic atypia, Toker cells are negative or only faintly reactive for HER2. |
 |
|
|
| Glycogenated keratinocytes can also occasionally bring to mind the appearance of Paget cells. Reassuring features include their mid-dermal location, lack of atypia, and gradual transition to keratinocytes. (Glycogenated keratinocytes) |
 |
|
|
Breast Pathology