Difference between revisions of "Pleomorphic Lobular Carcinoma In-situ"
| Line 1: | Line 1: | ||
| − | __NOCACHE__{{DISPLAYTITLE: | + | __NOCACHE__{{DISPLAYTITLE:}} |
{{:TOC}} | {{:TOC}} | ||
| − | == | + | <br> |
| − | + | == Introduction == | |
| − | + | {{dxintro|Lobular Neoplasia: Pleomorphic Lobular Carcinoma In-situ|Pleomorphic lobular carcinoma in-situ usually does not give rise to clinical findings, although it can give rise to calcifications. Surgeons usually strive to excise regions containing pleomorphic lobular carcinoma in-situ; consequently, pathologists should evaluate the proximity of the neoplastic cells to the margins of specimens containing this lesion. It is unclear if irradiation ought to play a role in the primary treatment of this condition.|Lobular neoplasia represents a neoplastic proliferation of atypical, dishesive, nonpolarized epithelial cells growing in apparently discontinuous, scattered foci within the glandular tree. Pathologists divide lobular neoplasia into two categories based on the number of the neoplastic cells. Lobular carcinoma in situ (LCIS) constitutes the more florid proliferation and atypical lobular hyperplasia (ALH) the less pronounced version. Pathologists classify examples of LCIS showing extreme pleomorphism as pleomorphic lobular carcinoma in situ.|None|Like those in all forms of lobular neoplasia, the cells of pleomorphic lobular carcinoma in-situ appear nonpolarized, exhibit dishesion, and do not stain for E-cadherin. Unlike classic lobular neoplasia, the cells and their nuclei vary markedly in size and shape.|Haagensen Type B lobular carcinoma in-situ (minimal pleomorphism); high-grade ductal carcinoma in-situ (cohesion, polarization, presence of E cadherin)|Although pathologists classify certain neoplastic proliferations showing dishesion, absence of polarization, and extreme pleomorphism as pleomorphic lobular carcinoma in-situ, researchers have not established widely accepted, specific criteria to establish this diagnosis.|34-1 PLCIS2.jpg|The cells in pleomorphic lobular carcinoma in-situ show the usual findings of lobular neoplasia plus extreme pleomorphism.}} | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Examples showing only moderate pleomorphism may represent the so-called type B lobular carcinoma in-situ. Other examples with extreme pleomorphism may represent ductal carcinoma in-situ with loss of E-cadherin. Pathologists at MGH make the diagnosis of pleomorphic lobular carcinoma in-situ only rarely. | Examples showing only moderate pleomorphism may represent the so-called type B lobular carcinoma in-situ. Other examples with extreme pleomorphism may represent ductal carcinoma in-situ with loss of E-cadherin. Pathologists at MGH make the diagnosis of pleomorphic lobular carcinoma in-situ only rarely. | ||
{{img4|34-2 Type_B.jpg|34-3 PLCIS1.jpg|Haagensen type B lobular carcinoma in-situ|Pleomorphic lobular carcinoma in-situ}} | {{img4|34-2 Type_B.jpg|34-3 PLCIS1.jpg|Haagensen type B lobular carcinoma in-situ|Pleomorphic lobular carcinoma in-situ}} | ||
Revision as of 08:50, July 17, 2020
Contents
Introduction
Warning: Display title "<span style="color:#AF0C3E"><b><font size="5"><span style="background-color:; color:">Lobular Neoplasia: Pleomorphic Lobular Carcinoma In-situ</span></font></b></span>" overrides earlier display title "".
|
Definition: Pleomorphic lobular carcinoma in-situ usually does not give rise to clinical findings, although it can give rise to calcifications. Surgeons usually strive to excise regions containing pleomorphic lobular carcinoma in-situ; consequently, pathologists should evaluate the proximity of the neoplastic cells to the margins of specimens containing this lesion. It is unclear if irradiation ought to play a role in the primary treatment of this condition. Clinical Significance: Lobular neoplasia represents a neoplastic proliferation of atypical, dishesive, nonpolarized epithelial cells growing in apparently discontinuous, scattered foci within the glandular tree. Pathologists divide lobular neoplasia into two categories based on the number of the neoplastic cells. Lobular carcinoma in situ (LCIS) constitutes the more florid proliferation and atypical lobular hyperplasia (ALH) the less pronounced version. Pathologists classify examples of LCIS showing extreme pleomorphism as pleomorphic lobular carcinoma in situ. Gross Findings: None Microscopic Findings: Like those in all forms of lobular neoplasia, the cells of pleomorphic lobular carcinoma in-situ appear nonpolarized, exhibit dishesion, and do not stain for E-cadherin. Unlike classic lobular neoplasia, the cells and their nuclei vary markedly in size and shape. Differential Diagnosis: Haagensen Type B lobular carcinoma in-situ (minimal pleomorphism); high-grade ductal carcinoma in-situ (cohesion, polarization, presence of E cadherin) Discussion: Although pathologists classify certain neoplastic proliferations showing dishesion, absence of polarization, and extreme pleomorphism as pleomorphic lobular carcinoma in-situ, researchers have not established widely accepted, specific criteria to establish this diagnosis. |
 |
Examples showing only moderate pleomorphism may represent the so-called type B lobular carcinoma in-situ. Other examples with extreme pleomorphism may represent ductal carcinoma in-situ with loss of E-cadherin. Pathologists at MGH make the diagnosis of pleomorphic lobular carcinoma in-situ only rarely.
 |
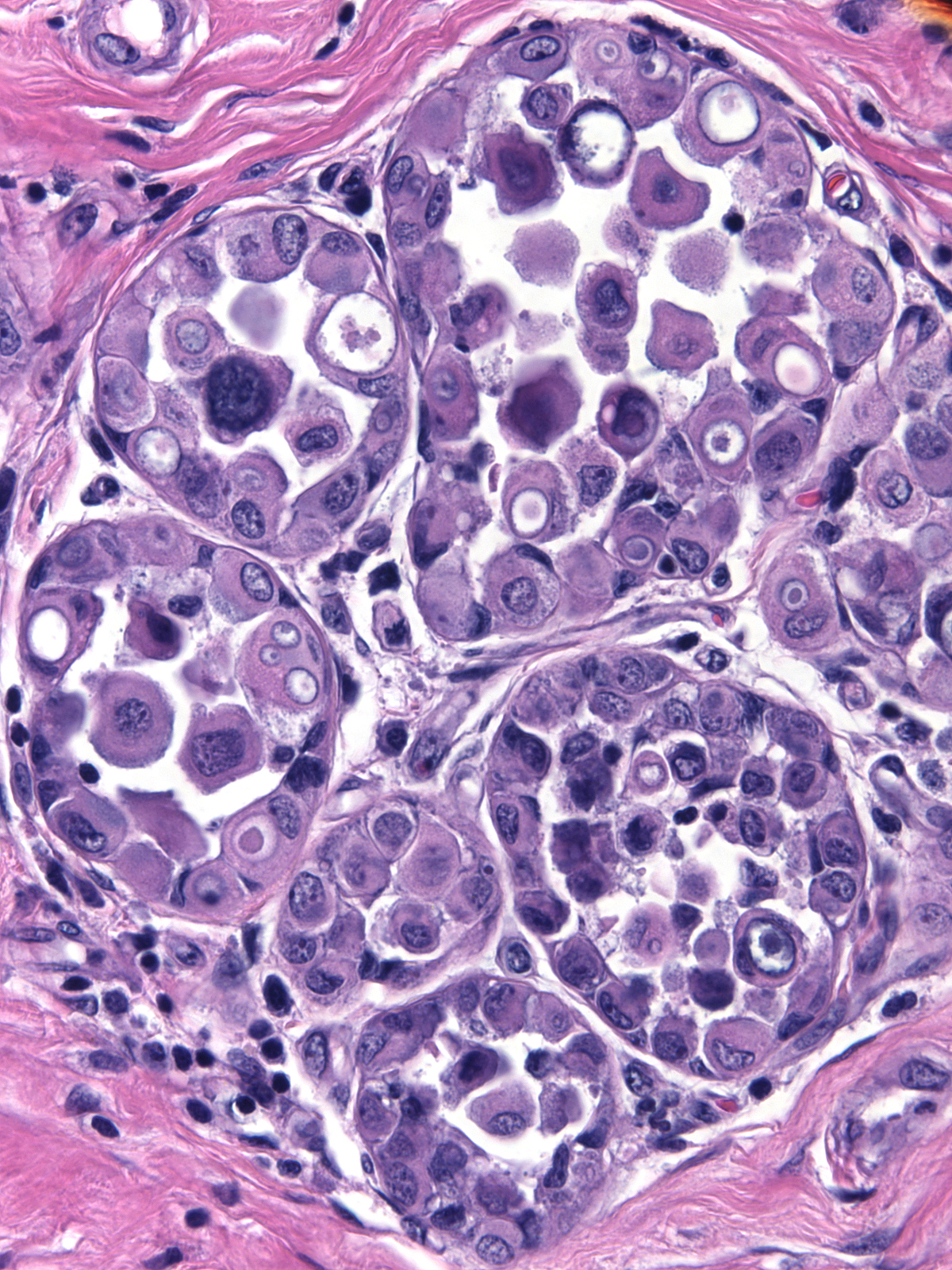 |
The cellular features of pleomorphic LCIS bring to mind those of high-grade DCIS growing in either conventional forms or a pagetoid manner. A search for evidence of cellular polarization and dishesion and staining for E-cadherin should reveal the nature of the neoplastic cells.
Specimens containing high-grade carcinomas in-situ frequently exhibit microinvasion, so one must search diligently for cells penetrating the stroma. Such foci usually reside in the immediate vicinity of the high-grade, non-invasive proliferation. The discovery of an invasive carcinoma is of much greater practical importance than distinguishing pleomorphic LCIS from high-grade DCIS.