Difference between revisions of "mgh:breast-Invasive Ductal Carcinoma (IDC)"
| Line 1: | Line 1: | ||
| − | __NOCACHE__ | + | __NOCACHE__ |
{{:TOC}} | {{:TOC}} | ||
| − | == | + | == Introduction == |
| − | + | {{dxintronodisc|Invasive Ductal Carcinoma (IDC)|Invasive ductal carcinoma (IDC), the most common type of breast cancer, is an adenocarcinoma composed of cells resembling mammary luminal cells. Most examples of invasive ductal carcinoma do not exhibit distinctive characteristics, and are referred to as "not otherwise specified" or simply "NOS". Carcinomas with specific growth patterns or morphological features belong in separate categories and represent subtypes of ductal carcinoma. Examples of special subtypes of ductal carcinoma include papillary carcinoma, mucinous carcinoma, and tubular carcinoma, among others.|Invasive ductal carcinoma usually presents as a mass evident on clinical examination or imaging studies. Most examples have the potential to kill the patient, although rare subtypes such as tubular carcinoma and adenoid cystic carcinoma virtually never do so. When a core biopsy reveals invasive ductal carcinoma, a surgeon will most often carry out excisions of the targeted region, marginal tissue, and the sentinel lymph node. In the following situations, the surgeon would carry out a mastectomy and sentinel node excision: recurrence of carcinoma in a breast previously treated with excision and irradiation, the presence of carcinoma at two separate sites in the breast, and carcinoma in a patient whose family history or genetic testing indicates a heightened risk for the development of breast cancer.|A typical invasive ductal carcinoma forms an irregular, poorly defined mass that feels firm or hard and consists of a mixture of white, tan, and pale yellow tissue (see basic gross pathology page).|Invasive ductal carcinoma consists of loosely cohesive aggregates of neoplastic cells growing beyond the basement membrane of the glandular tree. All but the least differentiated examples show evidence of glandular differentiation. The cytological characteristics vary depending on the grade of the carcinoma, but cytologic features common to most types of invasive ductal carcinoma include: enlargement of the cells with an increase in both the amount of the cytoplasm and the size of the nucleus; alteration in the quality of the chromatin; and cellular and nuclear pleomorphism. Mitotic figures and nucleolar aberrations are also common. For a description of the common cytologic features for each grade of carcinoma, see the Grading Invasive Carcinoma page.|Sclerosing adenosis (lobulated, zonal organization, intact basement membrane), radial scar (targetoid organization, usually intact myoepithelial layer)|10-1 idc_title_image.jpg|As its name suggests, invasive ductal carcinoma shares some morphologic features with normal mammary glands.}} | |
| − | |||
| − | |||
| − | Most examples of invasive ductal carcinoma do not exhibit distinctive characteristics, and are referred to as "not otherwise specified" or simply "NOS". Carcinomas with specific growth patterns or morphological features belong in separate categories and represent subtypes of ductal carcinoma. Examples of special subtypes of ductal carcinoma include papillary carcinoma, mucinous carcinoma, and tubular carcinoma, among others. | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
== Growth Patterns of IDC == | == Growth Patterns of IDC == | ||
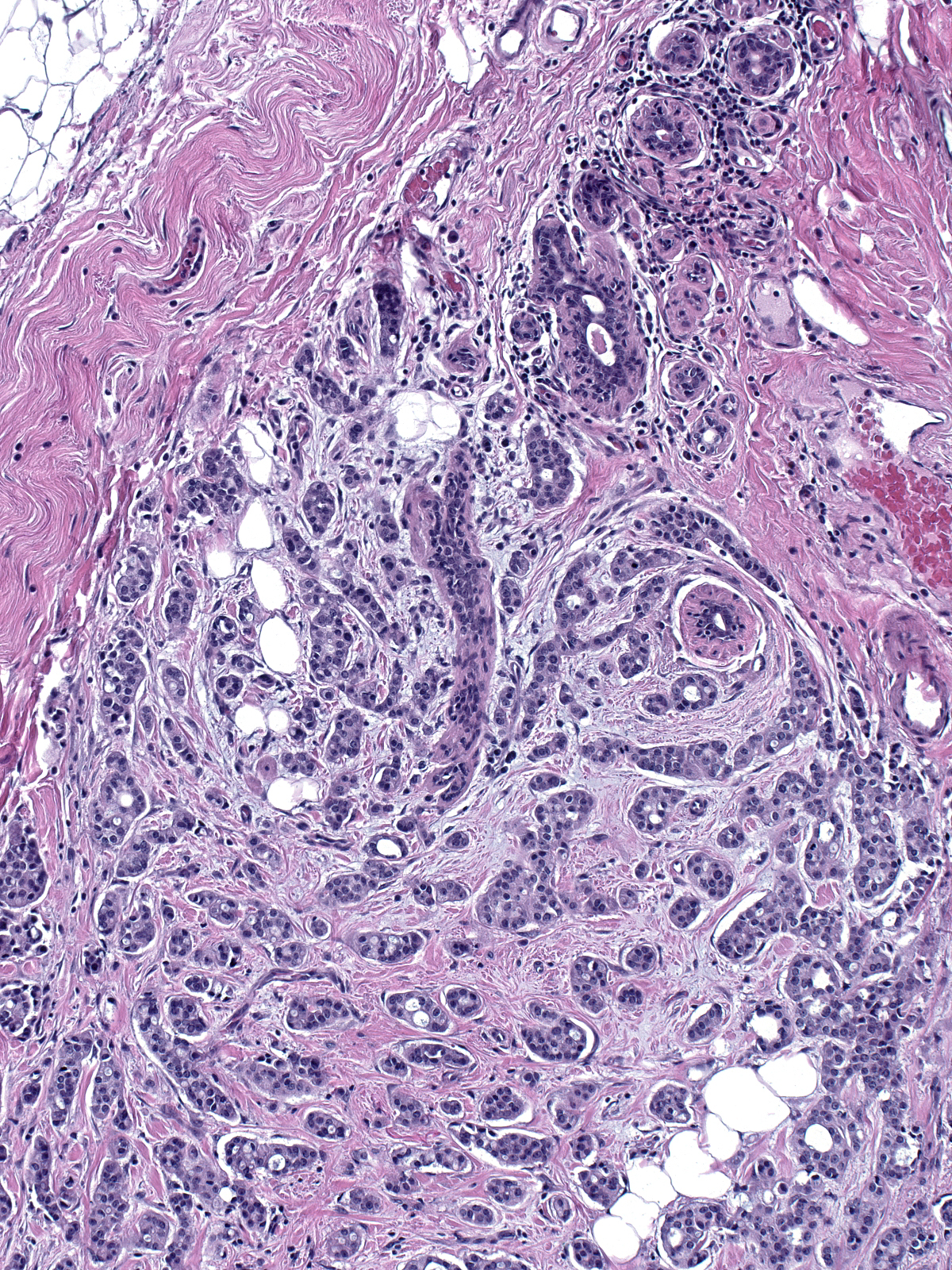
{{img1|Invasive ductal carcinomas exhibit a broad range of growth patterns. In the most common form, the cells create a compact mass consisting of both carcinoma cells and reactive stroma, which obliterate the underlying tissue.|10-2 Typical-2.jpg}} | {{img1|Invasive ductal carcinomas exhibit a broad range of growth patterns. In the most common form, the cells create a compact mass consisting of both carcinoma cells and reactive stroma, which obliterate the underlying tissue.|10-2 Typical-2.jpg}} | ||
Revision as of 17:56, July 16, 2020
Contents
Introduction
|
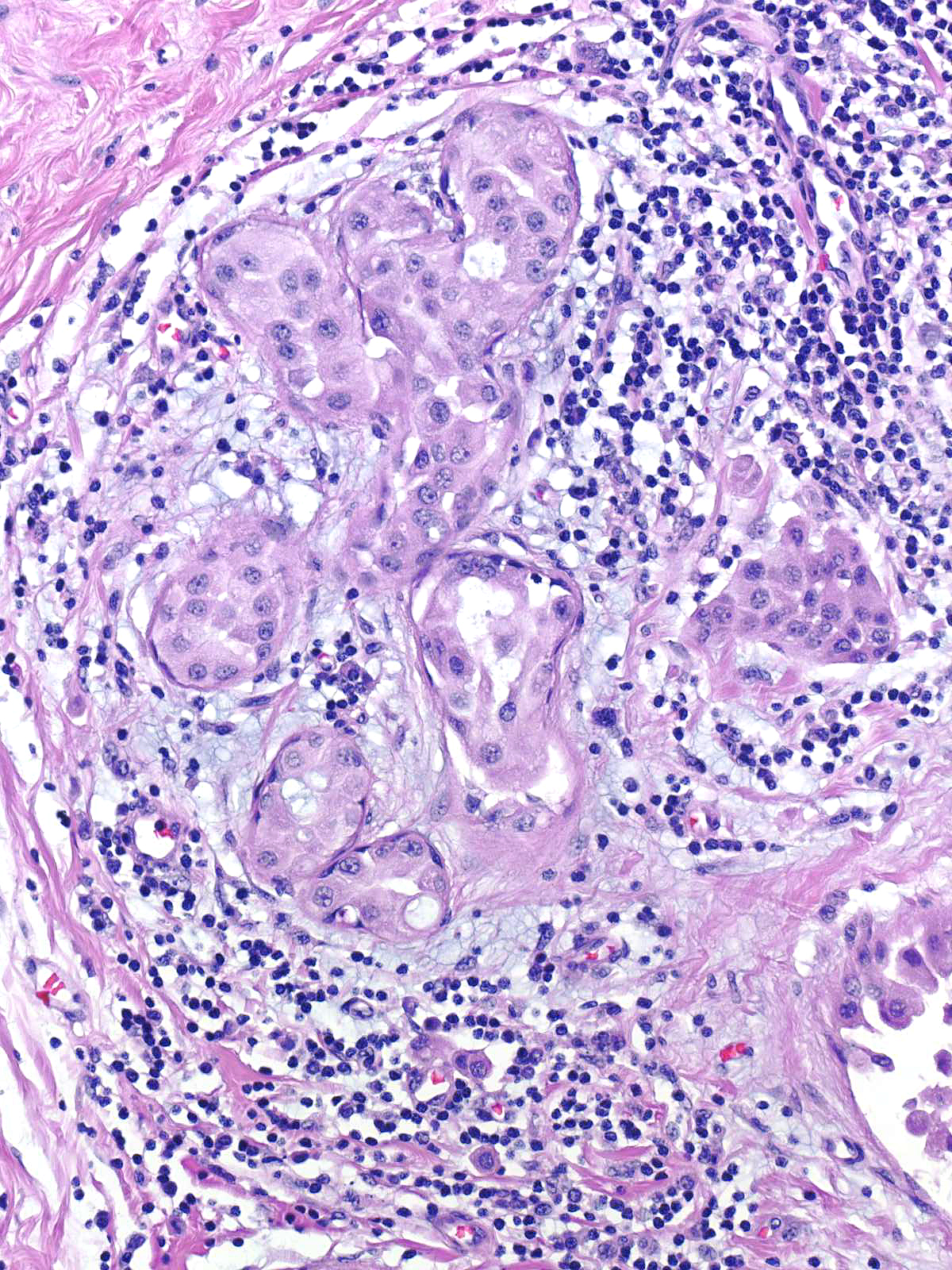
Definition: Invasive ductal carcinoma (IDC), the most common type of breast cancer, is an adenocarcinoma composed of cells resembling mammary luminal cells. Most examples of invasive ductal carcinoma do not exhibit distinctive characteristics, and are referred to as "not otherwise specified" or simply "NOS". Carcinomas with specific growth patterns or morphological features belong in separate categories and represent subtypes of ductal carcinoma. Examples of special subtypes of ductal carcinoma include papillary carcinoma, mucinous carcinoma, and tubular carcinoma, among others. Clinical Significance: Invasive ductal carcinoma usually presents as a mass evident on clinical examination or imaging studies. Most examples have the potential to kill the patient, although rare subtypes such as tubular carcinoma and adenoid cystic carcinoma virtually never do so. When a core biopsy reveals invasive ductal carcinoma, a surgeon will most often carry out excisions of the targeted region, marginal tissue, and the sentinel lymph node. In the following situations, the surgeon would carry out a mastectomy and sentinel node excision: recurrence of carcinoma in a breast previously treated with excision and irradiation, the presence of carcinoma at two separate sites in the breast, and carcinoma in a patient whose family history or genetic testing indicates a heightened risk for the development of breast cancer. Gross Findings: A typical invasive ductal carcinoma forms an irregular, poorly defined mass that feels firm or hard and consists of a mixture of white, tan, and pale yellow tissue (see basic gross pathology page). Microscopic Findings: Invasive ductal carcinoma consists of loosely cohesive aggregates of neoplastic cells growing beyond the basement membrane of the glandular tree. All but the least differentiated examples show evidence of glandular differentiation. The cytological characteristics vary depending on the grade of the carcinoma, but cytologic features common to most types of invasive ductal carcinoma include: enlargement of the cells with an increase in both the amount of the cytoplasm and the size of the nucleus; alteration in the quality of the chromatin; and cellular and nuclear pleomorphism. Mitotic figures and nucleolar aberrations are also common. For a description of the common cytologic features for each grade of carcinoma, see the Grading Invasive Carcinoma page. Differential Diagnosis: Sclerosing adenosis (lobulated, zonal organization, intact basement membrane), radial scar (targetoid organization, usually intact myoepithelial layer) |
Growth Patterns of IDC
| Invasive ductal carcinomas exhibit a broad range of growth patterns. In the most common form, the cells create a compact mass consisting of both carcinoma cells and reactive stroma, which obliterate the underlying tissue. | 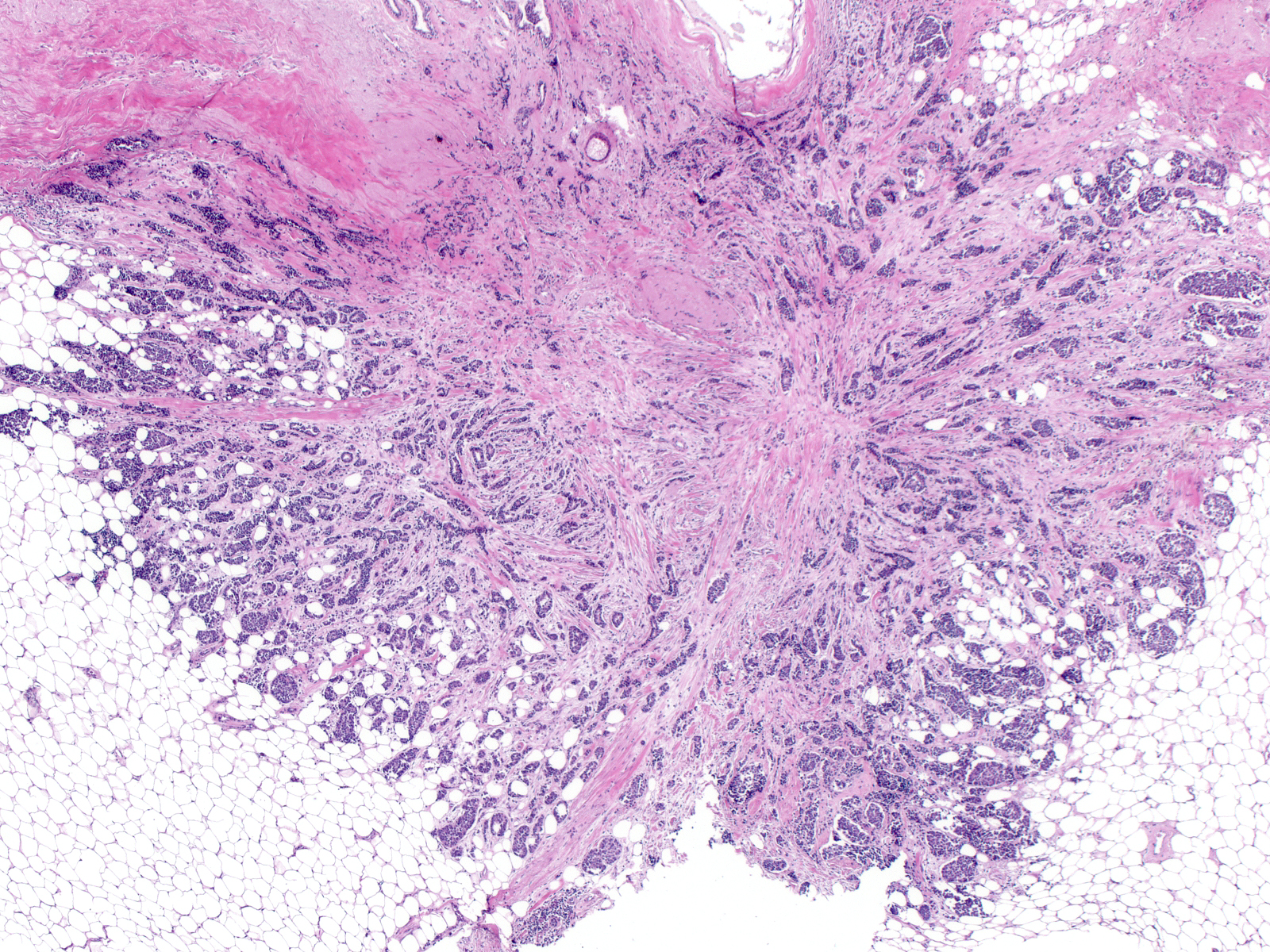 |
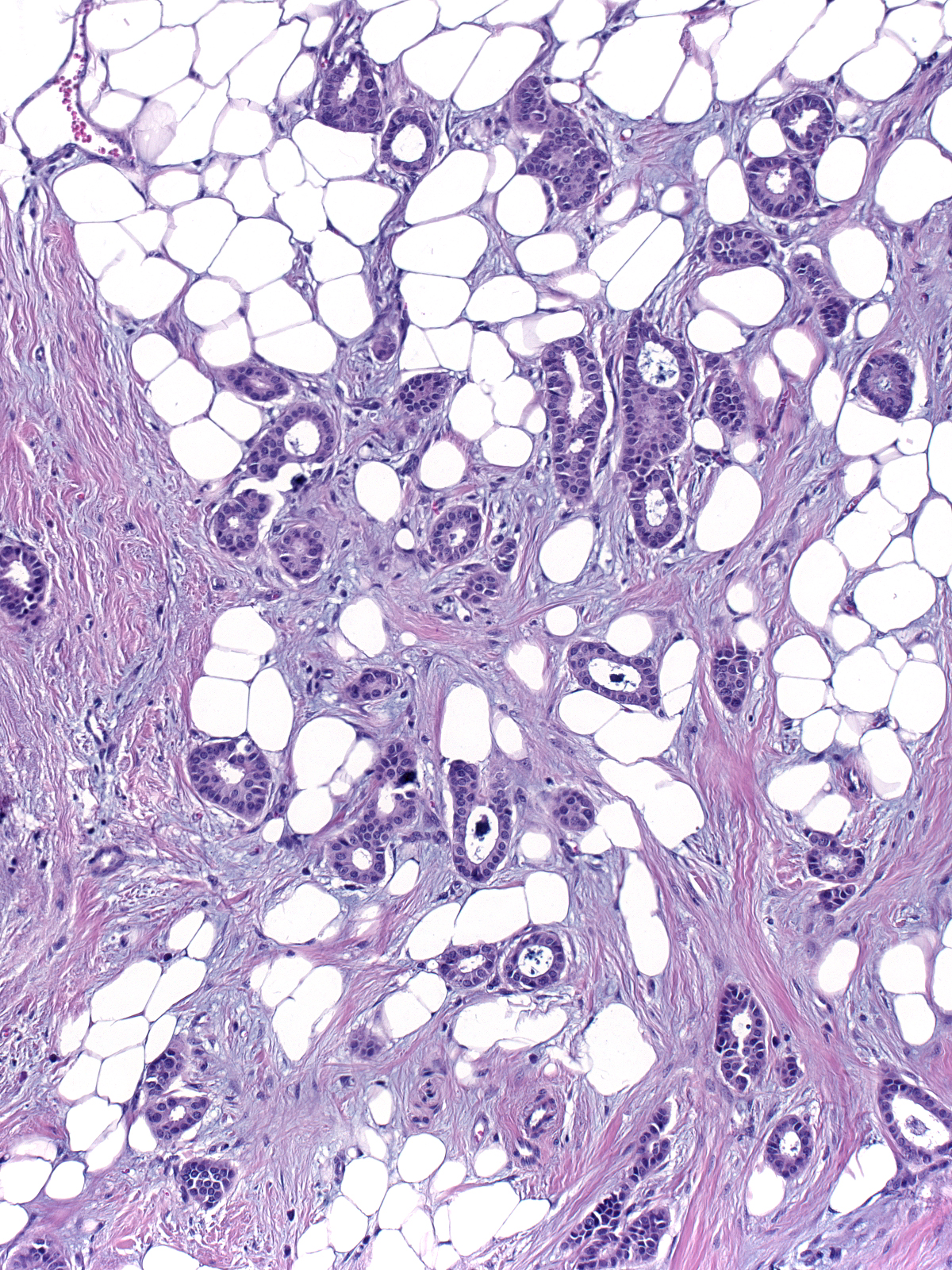
| In other cases, clusters of invasive cells infiltrate among pre-existing ducts and lobules without destroying them. | 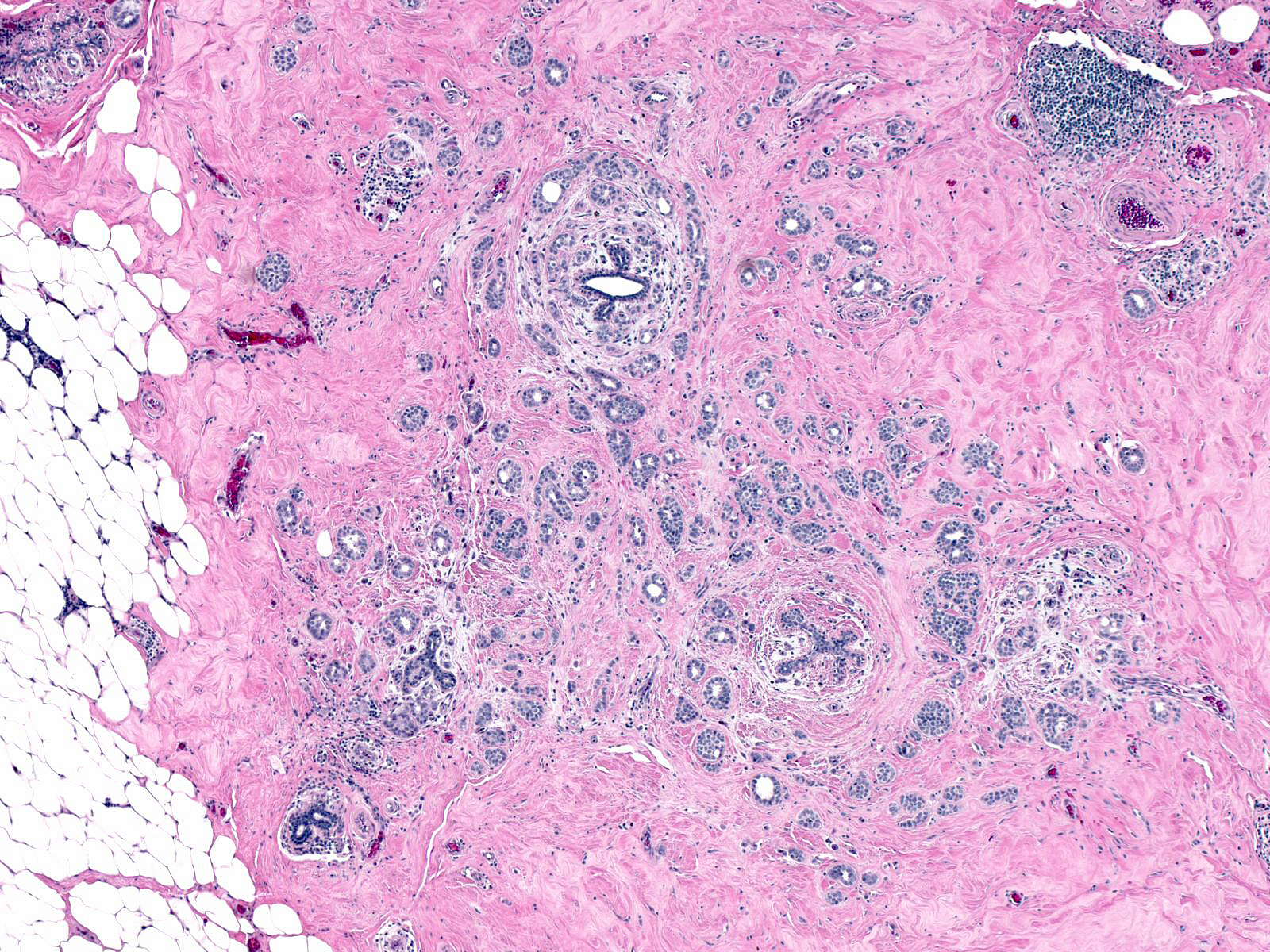 |
| IDCs can also feature slender chains of invasive cells that superficially resembles the single-file pattern of invasive lobular carcinoma. Unlike invasive lobular carcinoma, the ductal carcinoma cells are cohesive and focally exhibit polarization or even overt gland formation. | 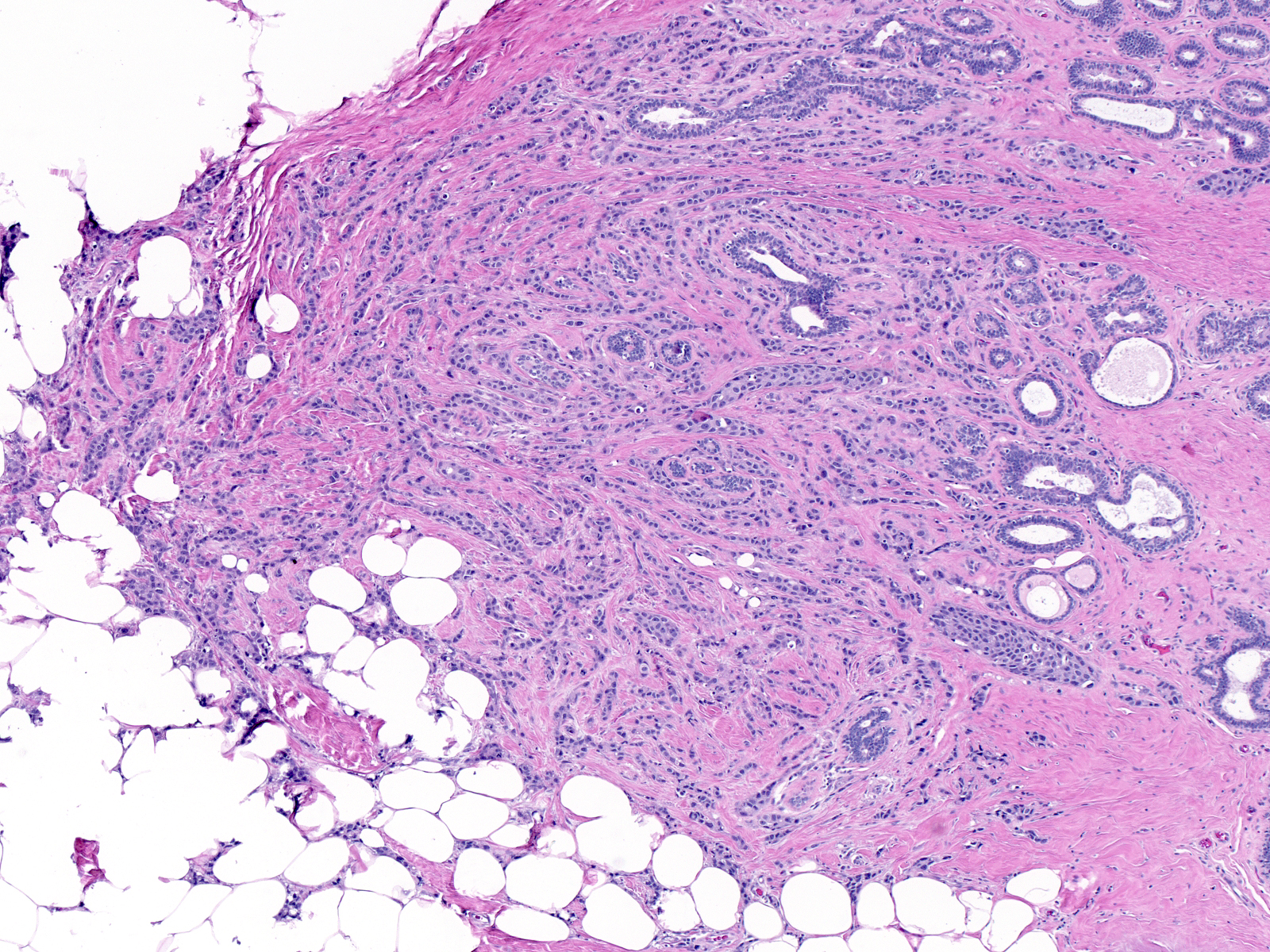 |
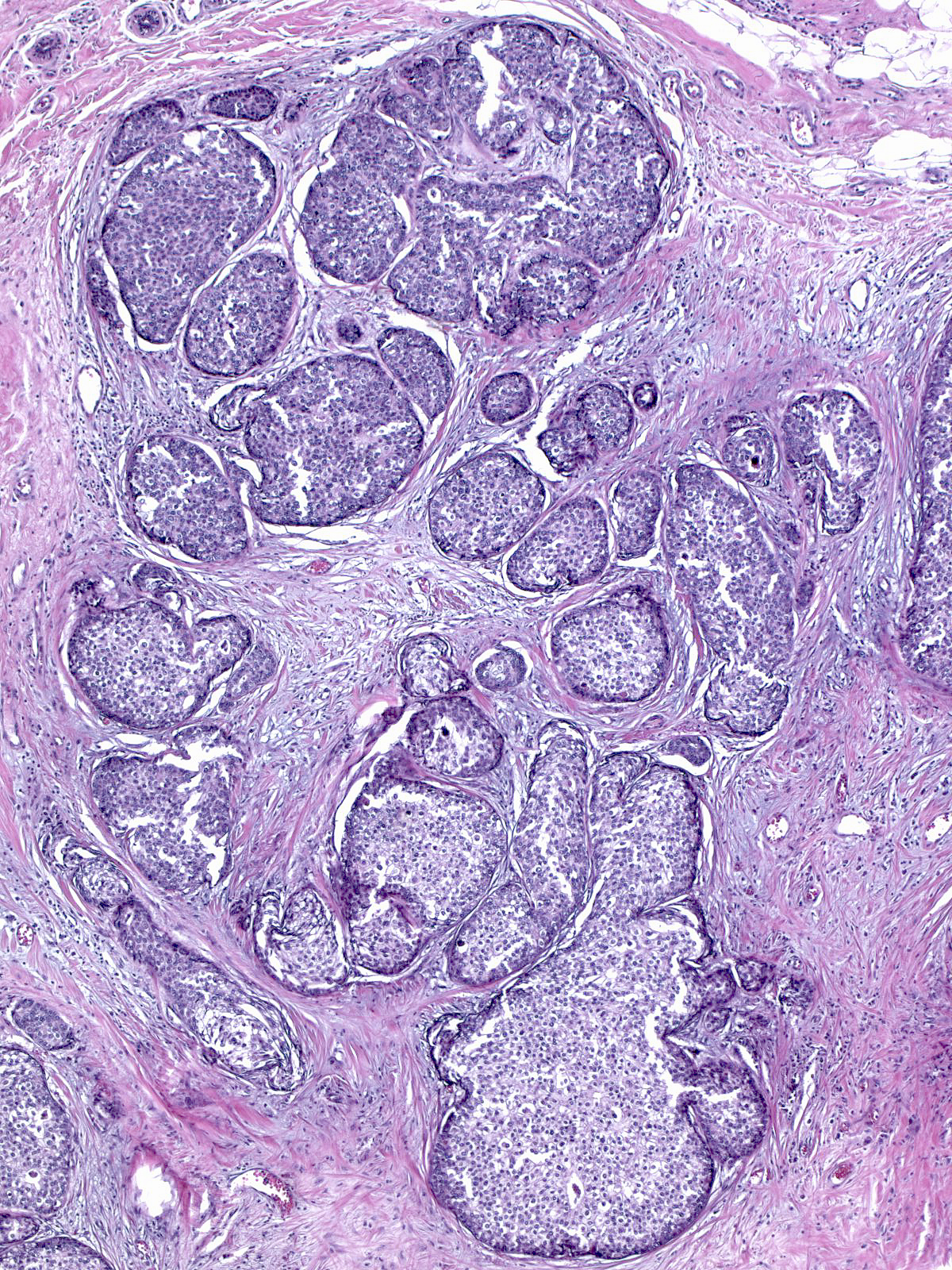
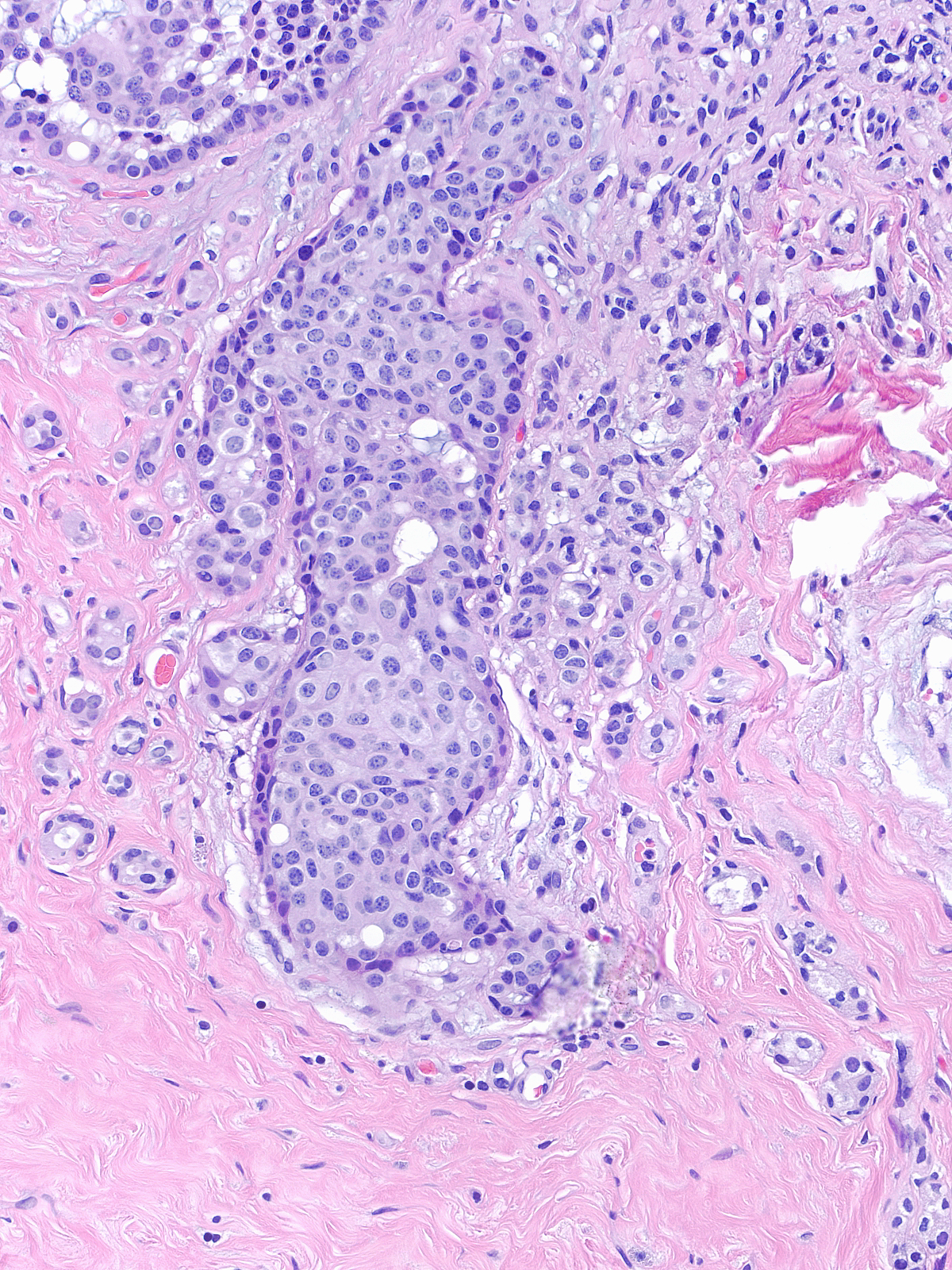
Some patterns are difficult to recognize as invasive. In the example on the left, the IDC is composed of large round nests of carcinoma cells that simulate glands distended by carcinoma in-situ. On the right, the IDC features a compact collection of glands that resemble a lobule.
 |
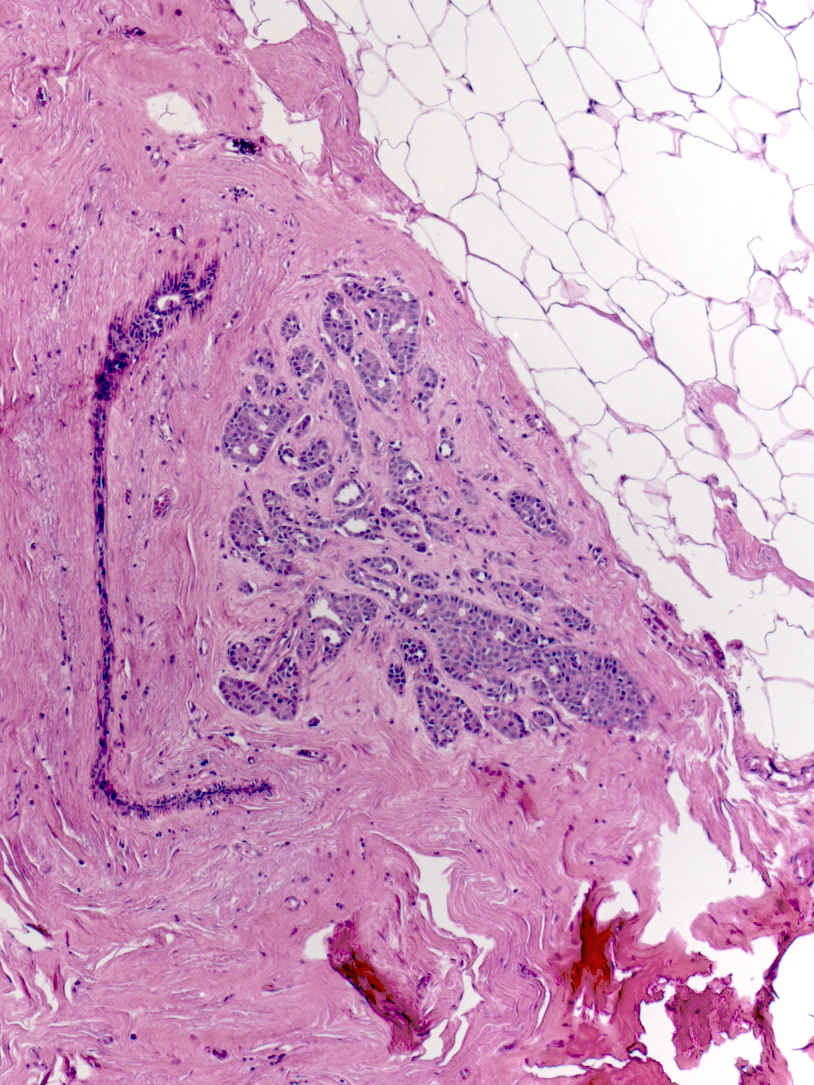 |
| Invasive ductal carcinoma can also resemble benign lesions. In this example, the IDC might be mistaken for adenosis. | 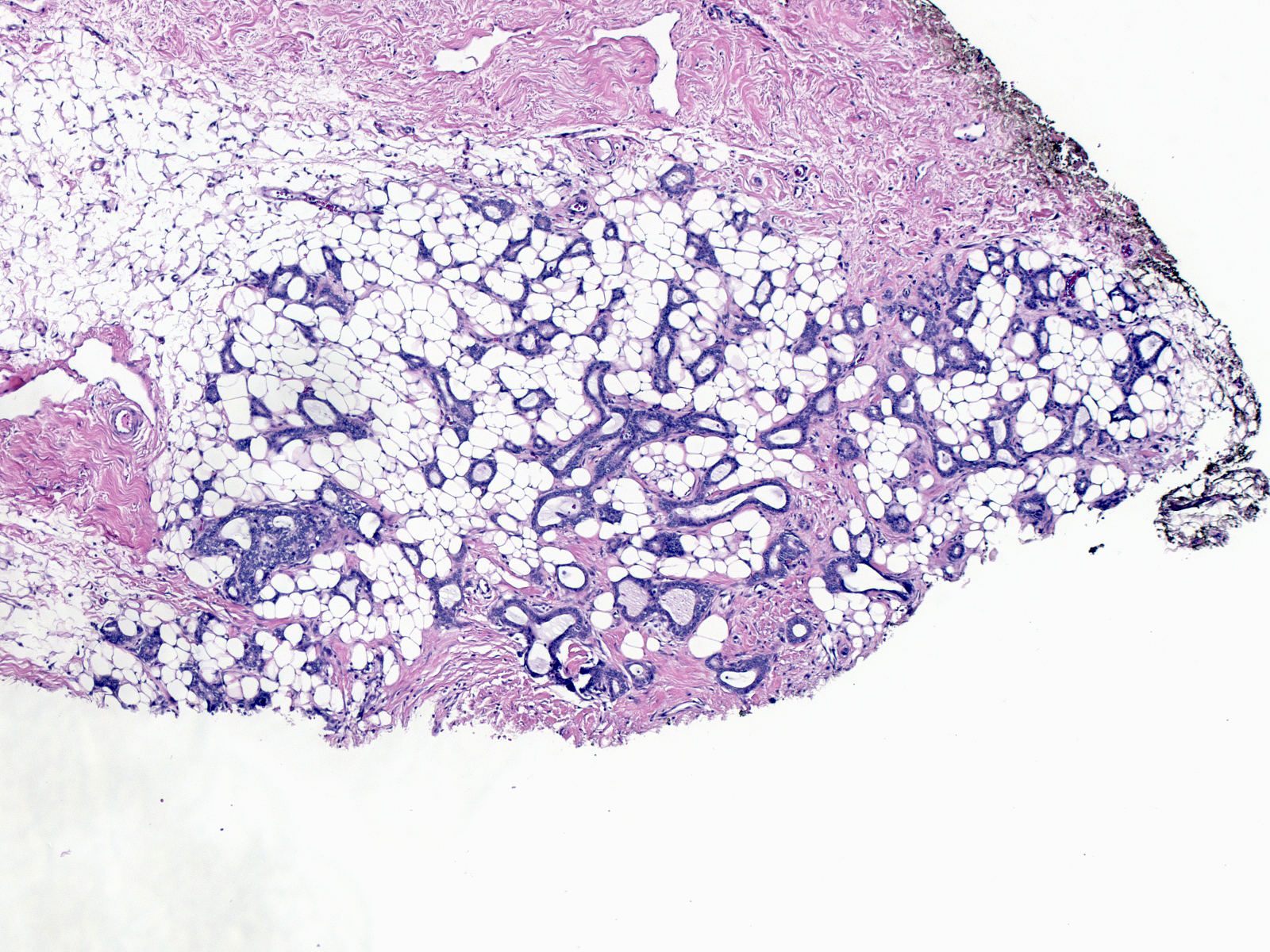 |
In particularly deceptive cases, the pattern consists of widely scattered clusters composed of just a few cells each.
 |
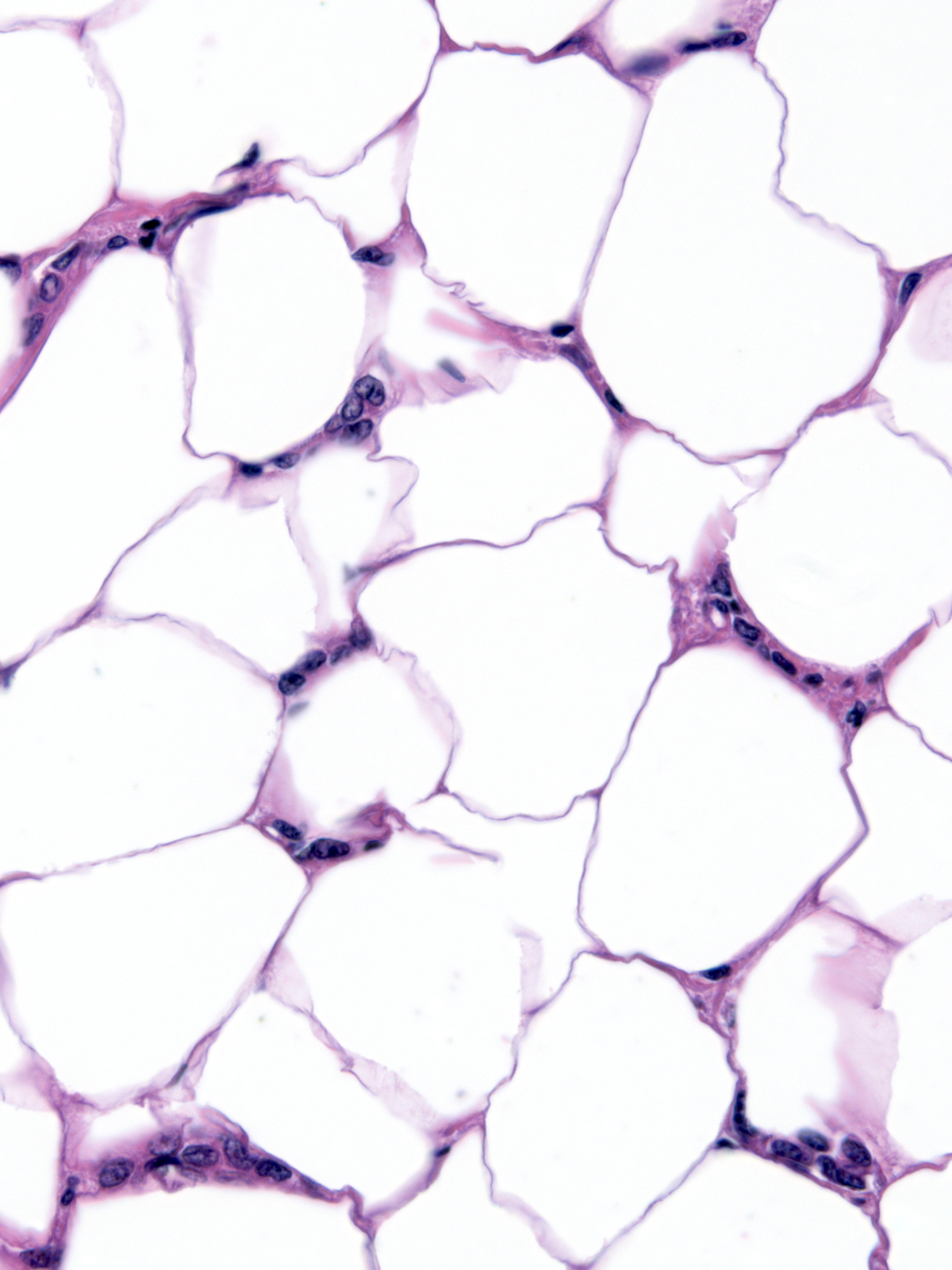 |
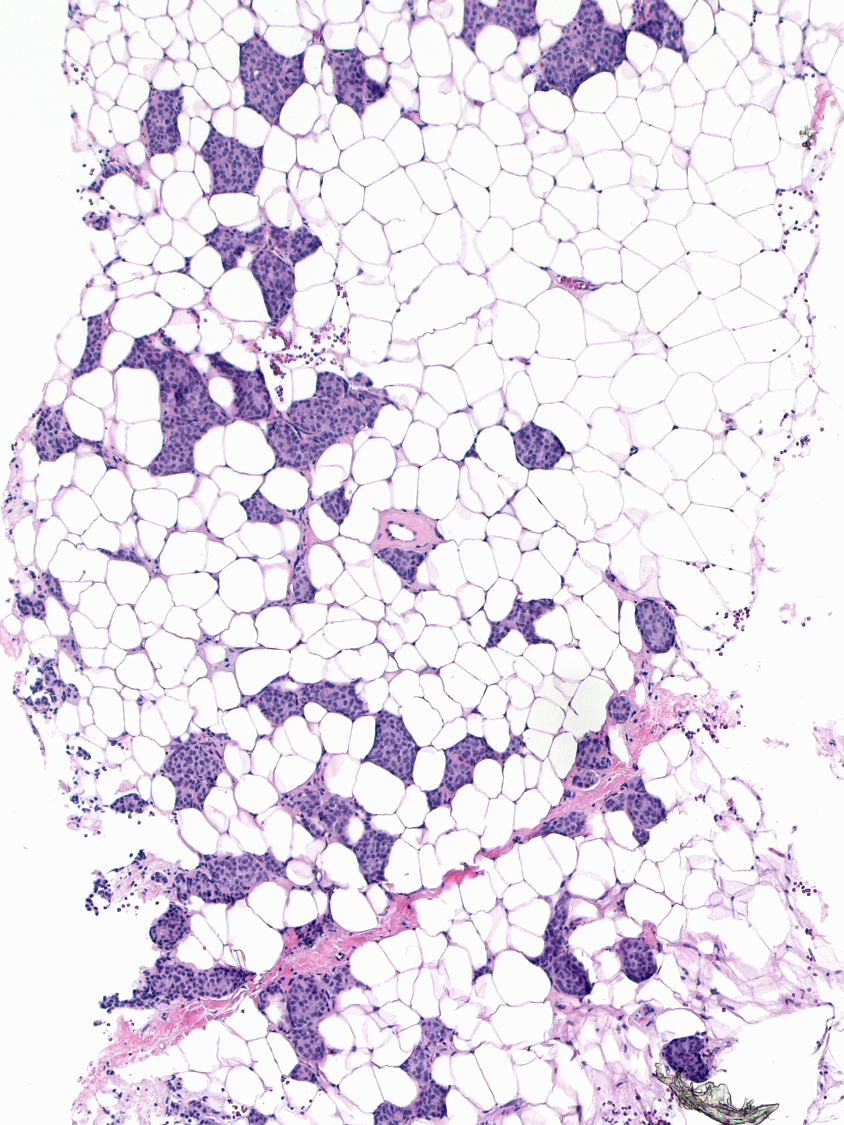
One could easily overlook these rare IDC cells nestled among the adipocytes.
Detection of IDC
To detect foci of invasion, look for clusters of epithelial cells that appear out-of-place or are infiltrating around normal structures. For example, take careful notice of epithelial cells encircling small ducts or blood vessels.
 |
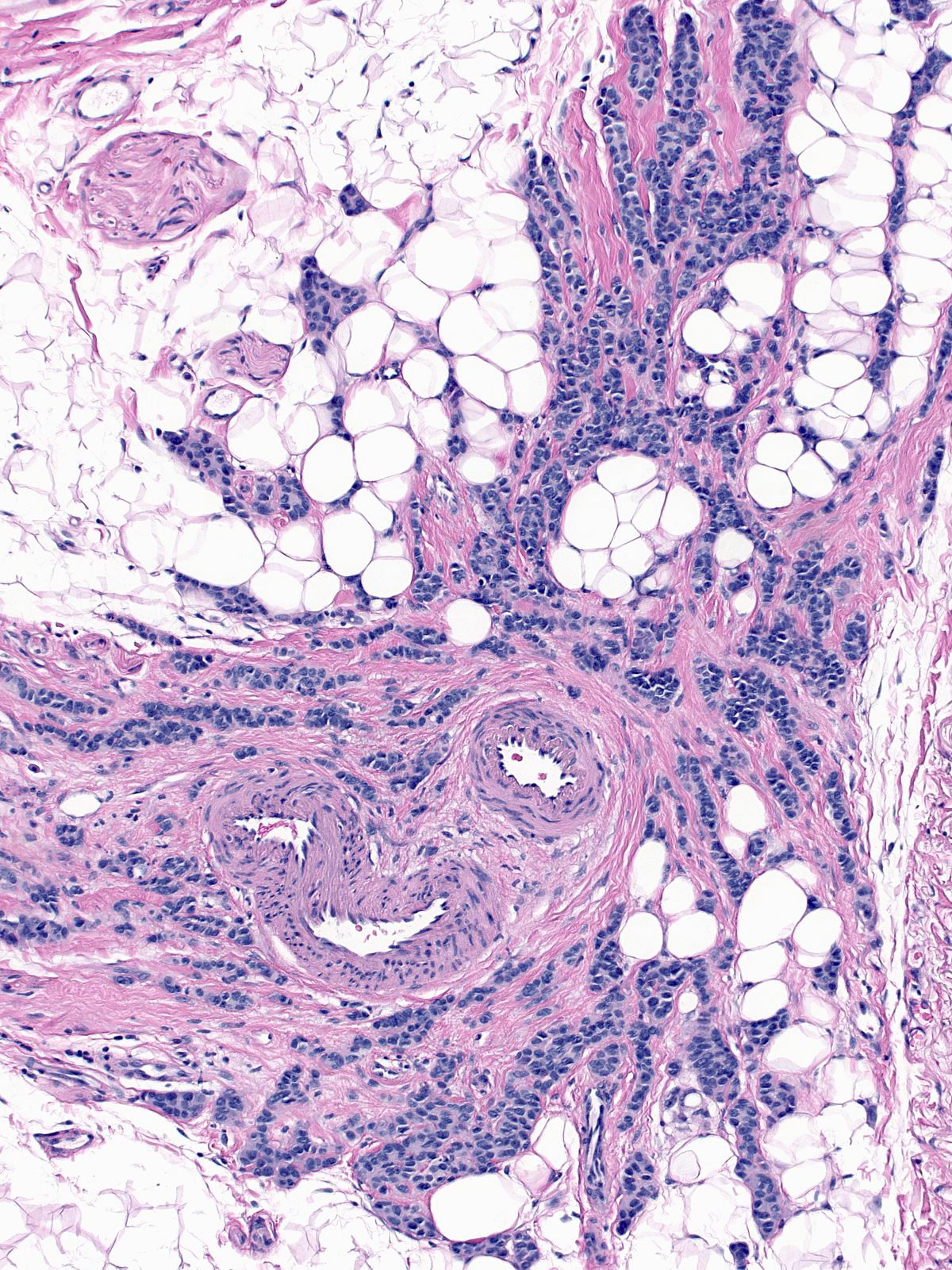 |
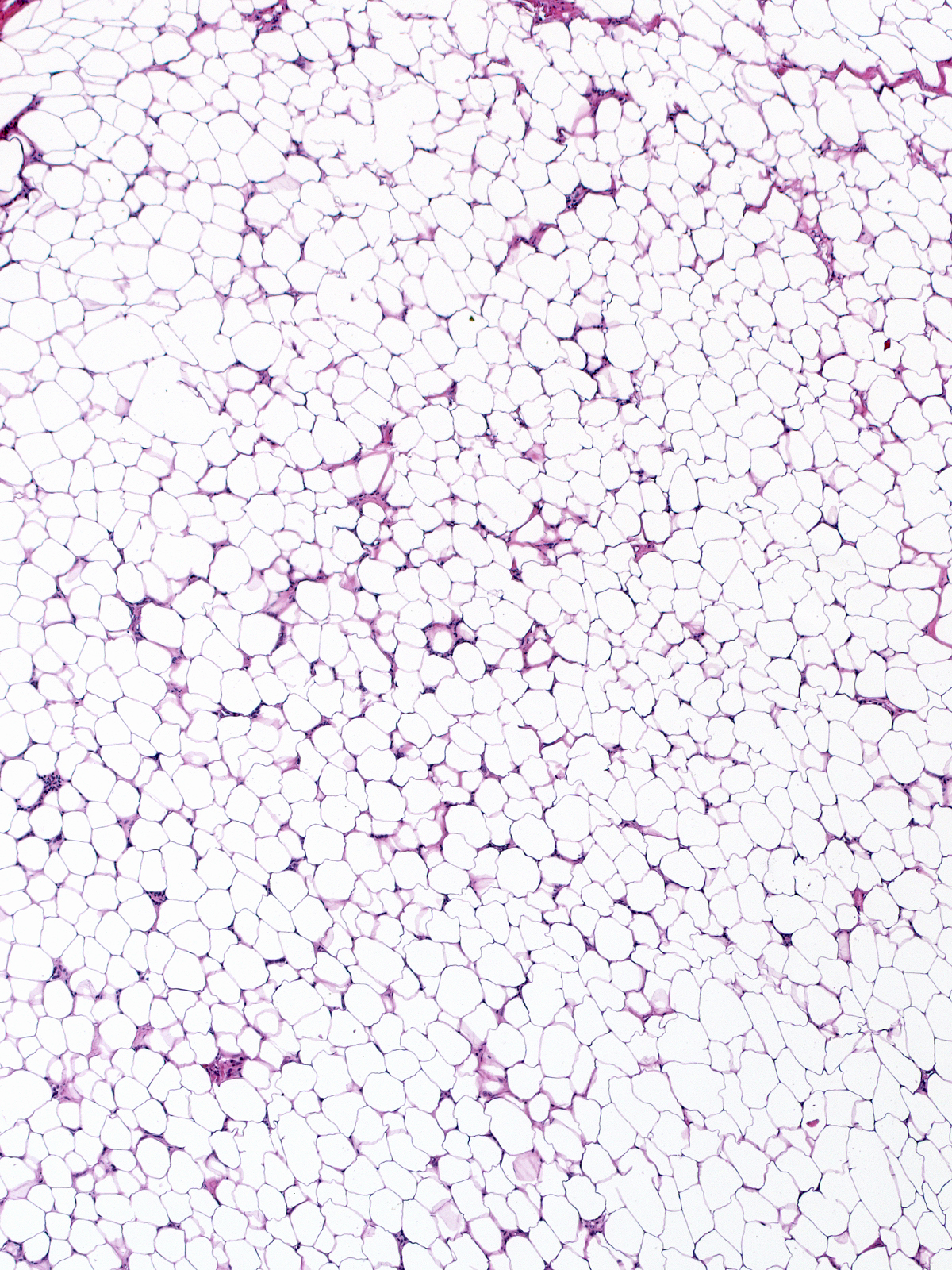
Equally alarming are epithelial cells penetrating benign lobules or invading fat. Remember the layered organization of the breast, epithelium and fat should never directly juxtapose.
 |
 |
| Look also for groups that do not display the arrangement of mammary glandular tissue or the smooth contours of ducts and acini. The glands in the photo to the right superficially resemble ductal carcinoma in-situ, but their distribution and irregular shapes suggest IDC. | 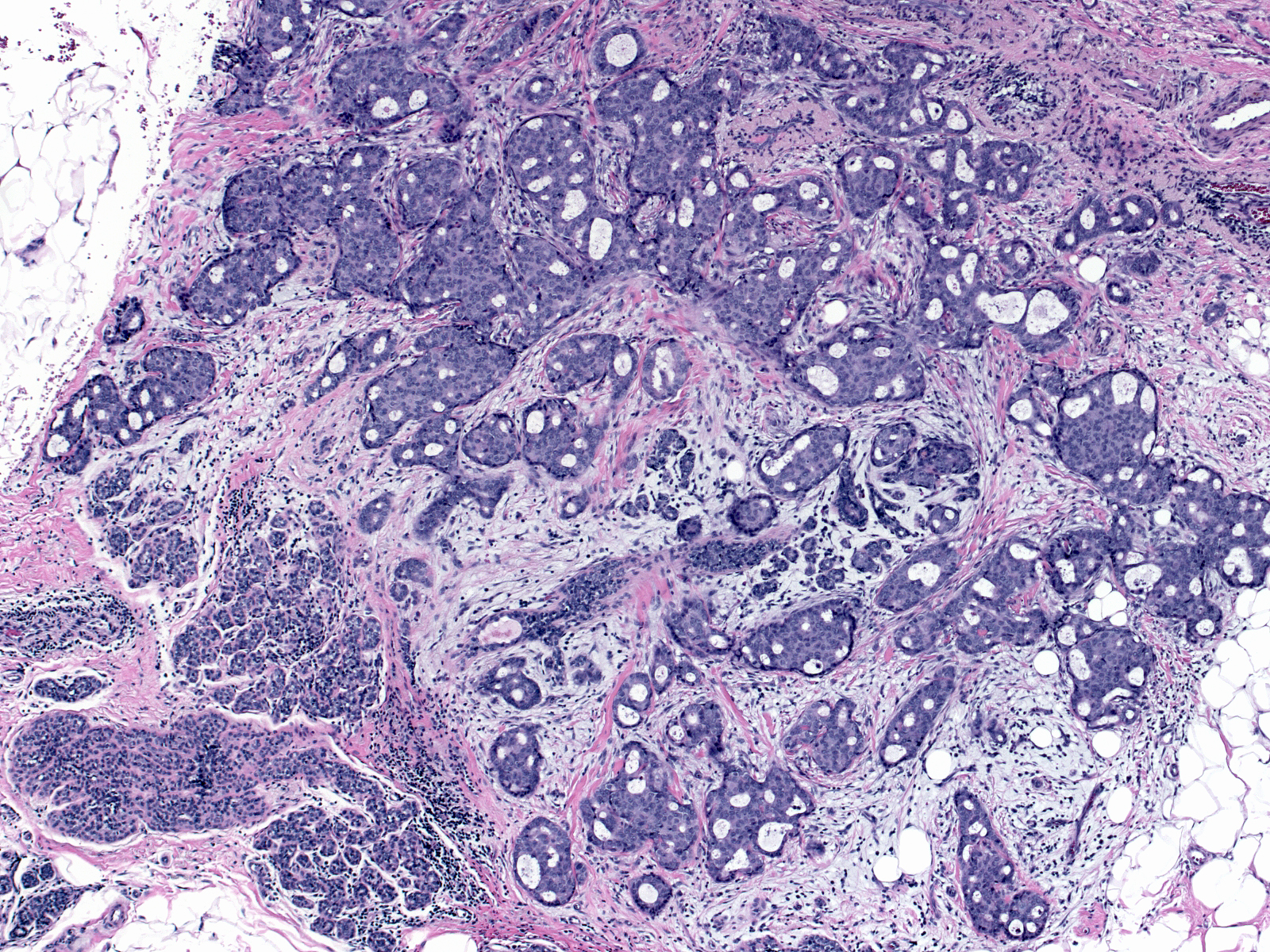 |
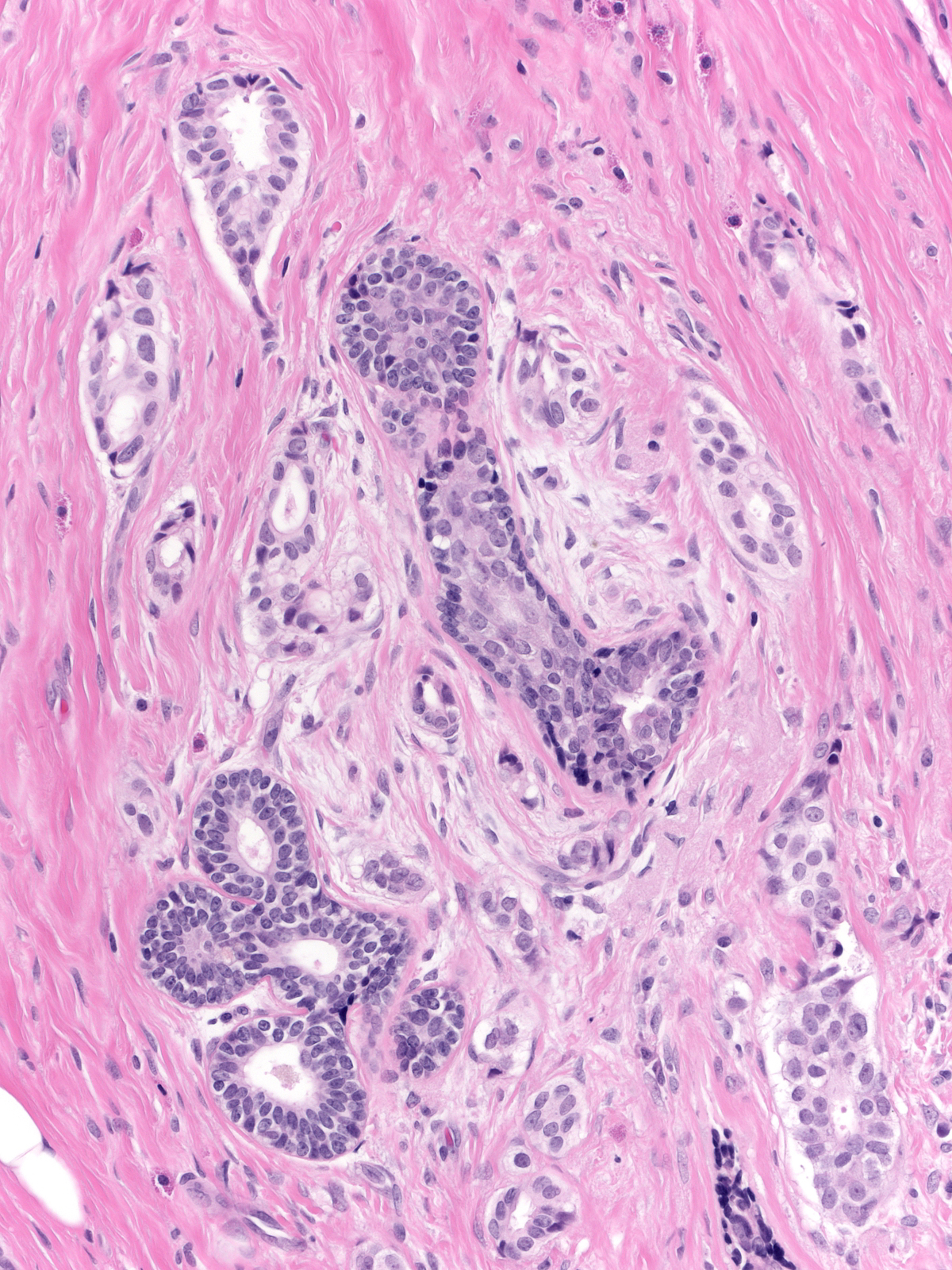
Pay close attention to the stroma. Invasive carcinomas frequently evoke a desmoplastic stromal reaction or a lymphocytic infiltration.
 |
 |
| Careful evaluation of the collagen structure can also be extremely helpful. Invasive cells disrupt the arrangement of collagen bundles. | 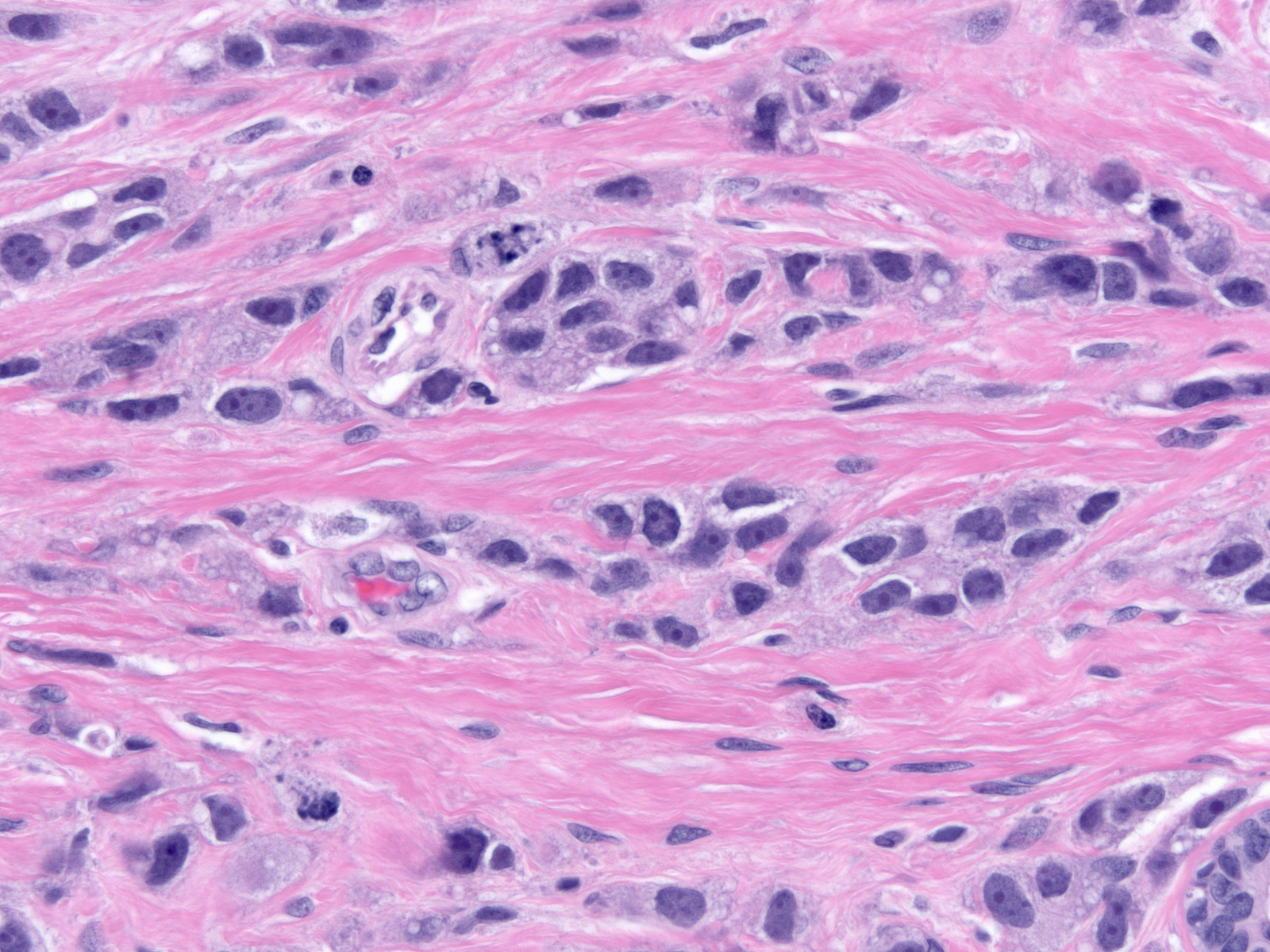 |
Microinvasion
Pathologists classify foci of invasive carcinoma spanning 0.1 cm or less as microinvasive.
 |
 |
Immunostaining helps in the detection and documentation of microinvasion. Stains for keratin often reveal invasive clusters and single cells nearly impossible to detect using H&E stains.
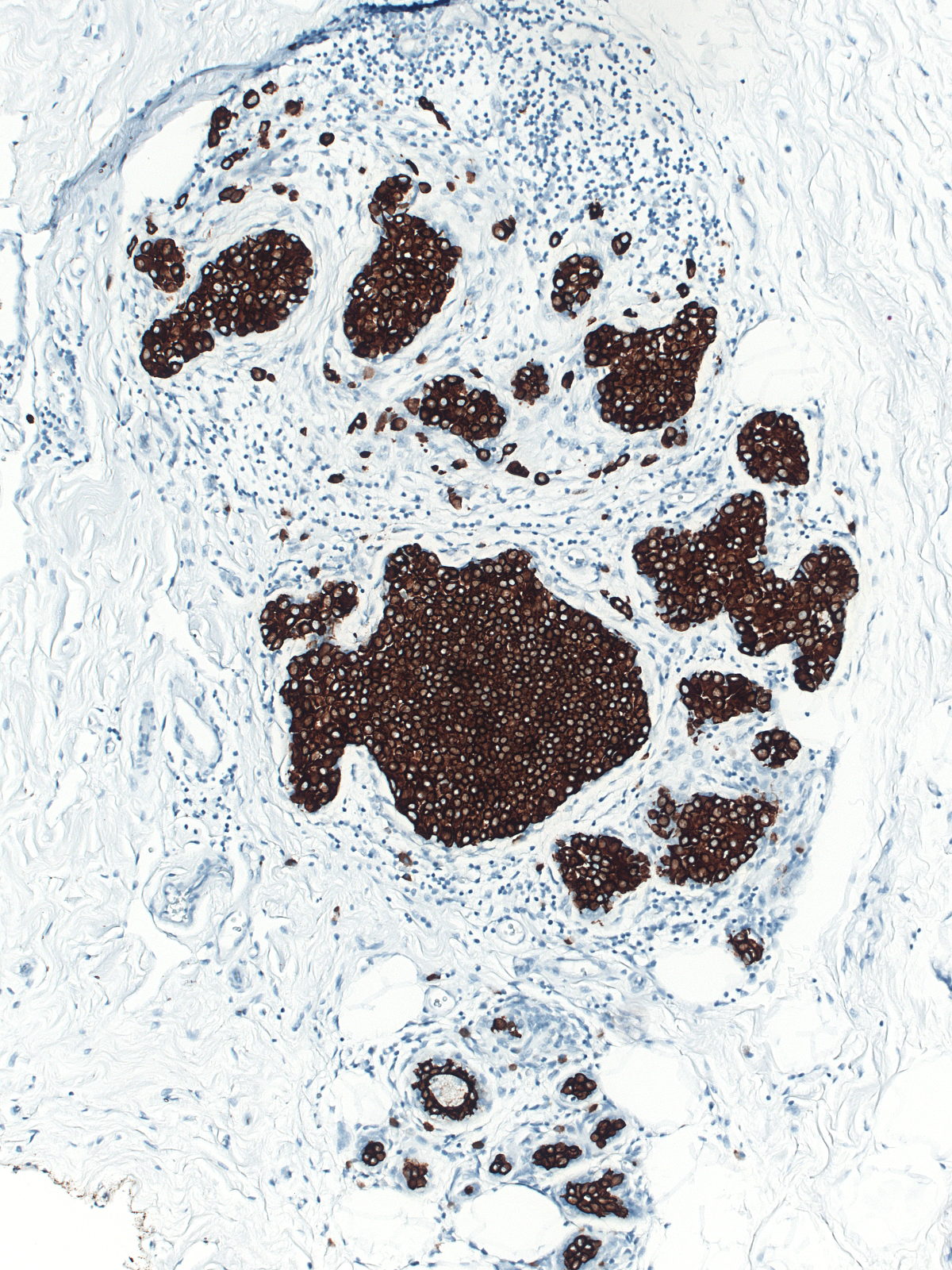 |
|
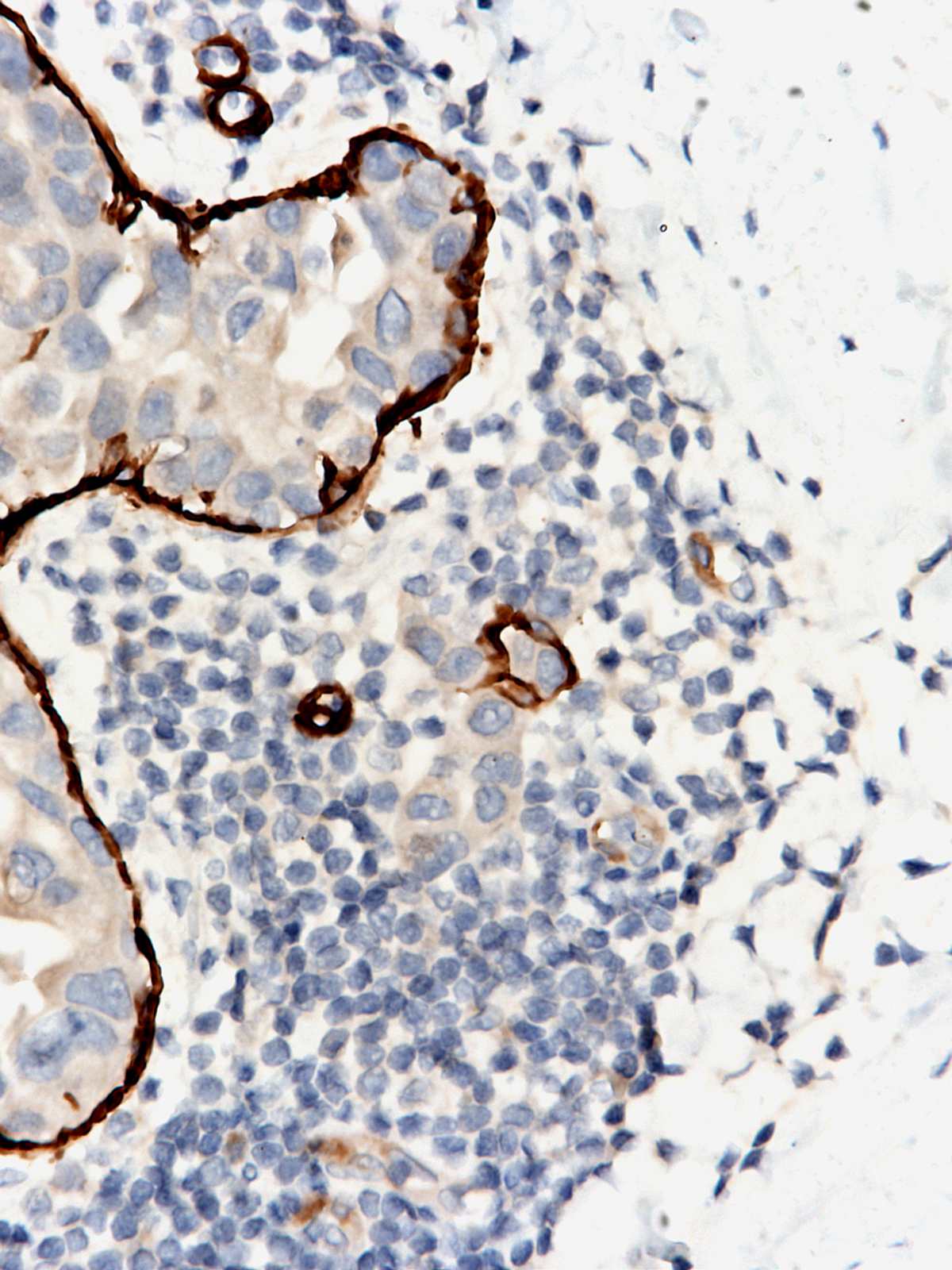
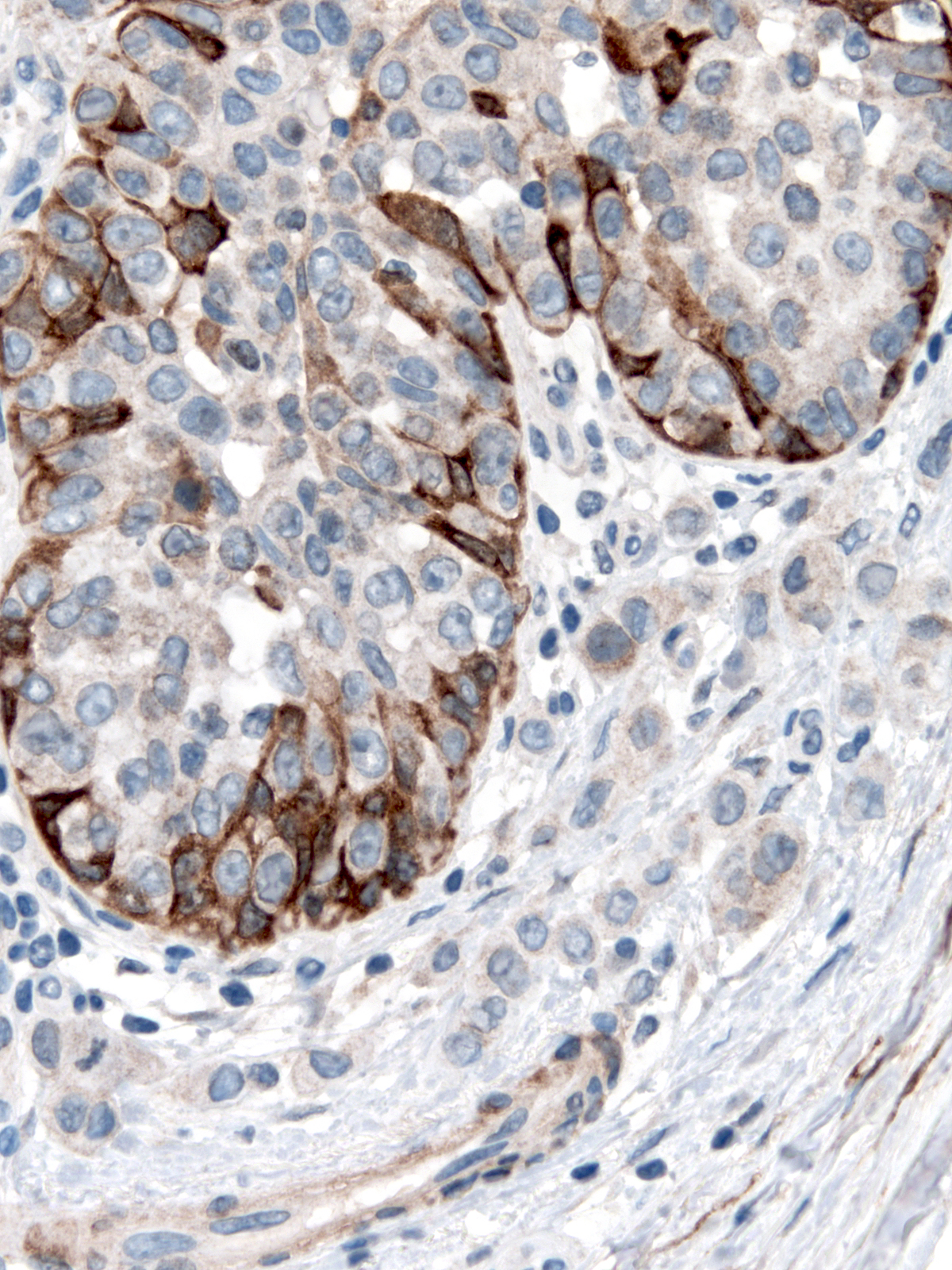
Stains for smooth muscle myosin heavy chain and calponin will demonstrate the absence of myoepithelial cells that characterize invasive nests.
 |
 |
| One occasionally finds cells penetrating the basement membrane but still attached to the cells within the ductule. Believing that invasive cells must not be in continuity with cells within the basement membrane, many pathologists would refrain from classifying such attached cells as invasive. | 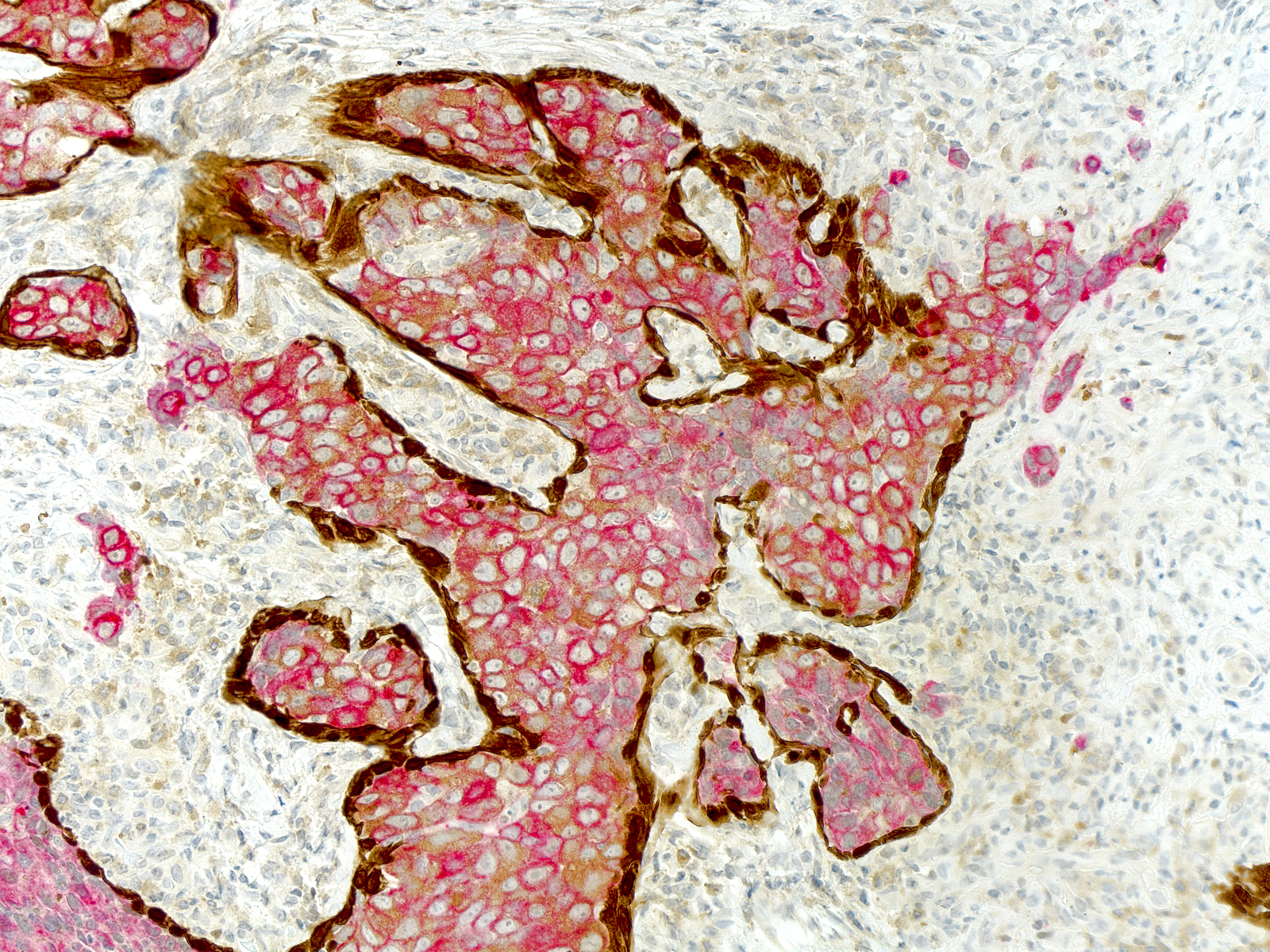 |
Combined immunostain showing carinoma in red (keratin) and myoepithelium in brown.
Differential Diagnosis
Sclerosing adenosis and radial scars both display characteristic patterns of organization not seen in invasive ductal carcinomas. Moreover, classic examples of these benign alterations do not feature cells with cytological atypia. Neoplastic ductal cells can populate glands altered by sclerosing adenosis and radial scars, thereby creating a resemblance to invasive carcinoma. Careful attention to the organization of the focus and the results of immunohistochemical stains will usually establish the noninvasive nature of such foci.