|
|
| Line 39: |
Line 39: |
| | {{img1|Many noninvasive carcinomas with a papillary architecture represent papillomas overrun by ductal carcinoma in-situ.|32-20 Papilloma_w_DCIS.jpg}} | | {{img1|Many noninvasive carcinomas with a papillary architecture represent papillomas overrun by ductal carcinoma in-situ.|32-20 Papilloma_w_DCIS.jpg}} |
| | {{img1|To establish this diagnosis, one must find evidence of the pre-existing papilloma. The presence of benign epithelium, a substantial number of myoepithelial cells, or histiocytes in the stromal cores usually substantiates the notion of an underlying papilloma. The presence of ductal carcinoma in-situ in adjoining ducts would add additional but less substantial evidence to support the diagnosis of papilloma overrun by ductal carcinoma in-situ.|32-21 Papilloma_frond.jpg}} | | {{img1|To establish this diagnosis, one must find evidence of the pre-existing papilloma. The presence of benign epithelium, a substantial number of myoepithelial cells, or histiocytes in the stromal cores usually substantiates the notion of an underlying papilloma. The presence of ductal carcinoma in-situ in adjoining ducts would add additional but less substantial evidence to support the diagnosis of papilloma overrun by ductal carcinoma in-situ.|32-21 Papilloma_frond.jpg}} |
| − | == Quiz ==
| + | {{:mgh:breast-footer}} |
| − | <bootstrap_collapse text="Start Quiz"><p><https://hub.partners.org/pathology/assessment/instructions?assessment_id=16607996" height="666" width="100%"></htmltag>
| |
| − | </p></bootstrap_collapse>
| |
Revision as of 18:16, July 13, 2020
General
Papillary carcinoma represents a type of invasive ductal carcinoma exhibiting a papillary architecture.
- Definition: Papillary carcinoma is a type of invasive ductal carcinoma in which the carcinoma cells grow on a fibrovascular skeleton.
- Clinical Significance: The carcinoma typically affects women older than 60 years. Many are beyond the age of 70 years. Conventional invasive papillary carcinoma accounts for a greater proportion of breast cancers in men than in women.
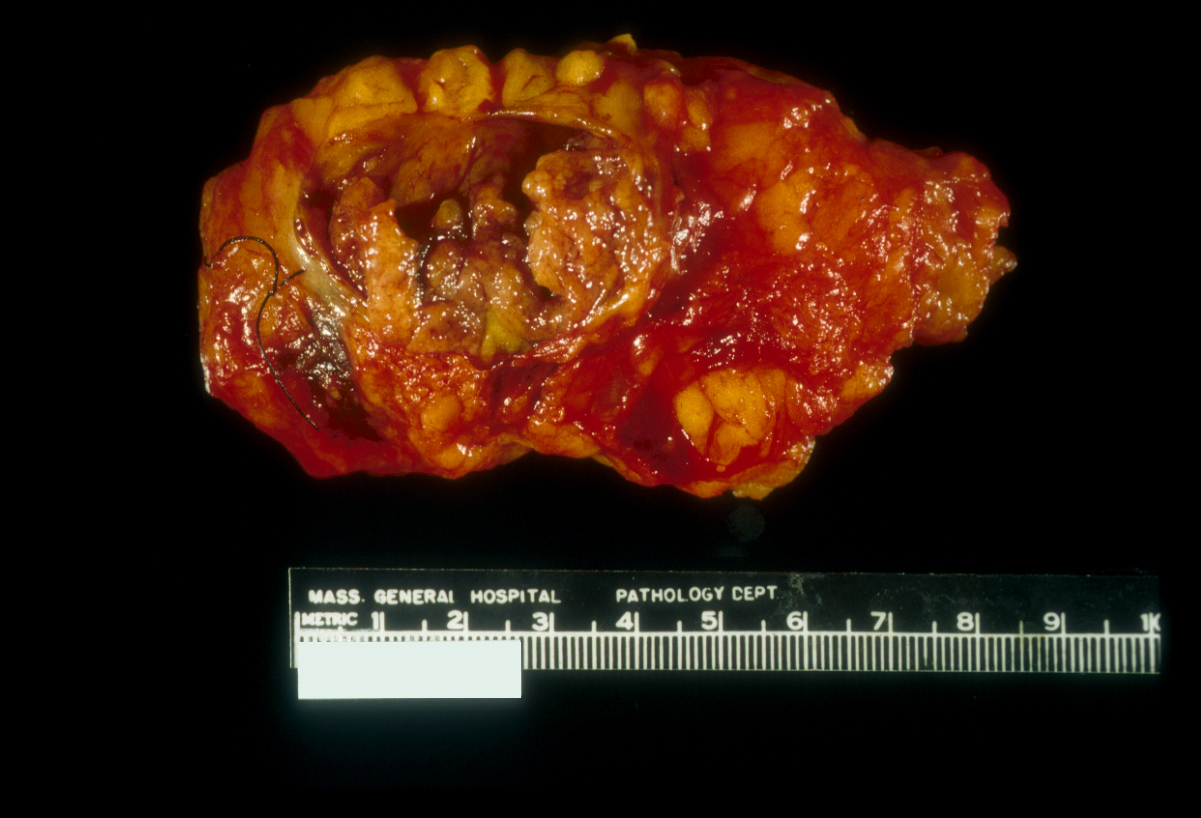
- Gross Findings: Papillary carcinoma usually forms a mostly well defined, irregular, mass composed of delicate friable, brown tissue, which often displays evidence of hemorrhage.
- Microscopic Findings: An arborizing scaffold of fibrovascular tissue supports the neoplastic ductal cells. Most conventional papillary carcinomas demonstrate invasion; purely non-invasive conventional papillary carcinomas occur only rarely. Typical invasive papillary carcinomas express estrogen receptors.
- Differential Diagnosis: Papilloma (no atypia), papilloma with carcinoma in-situ (underlying papilloma)
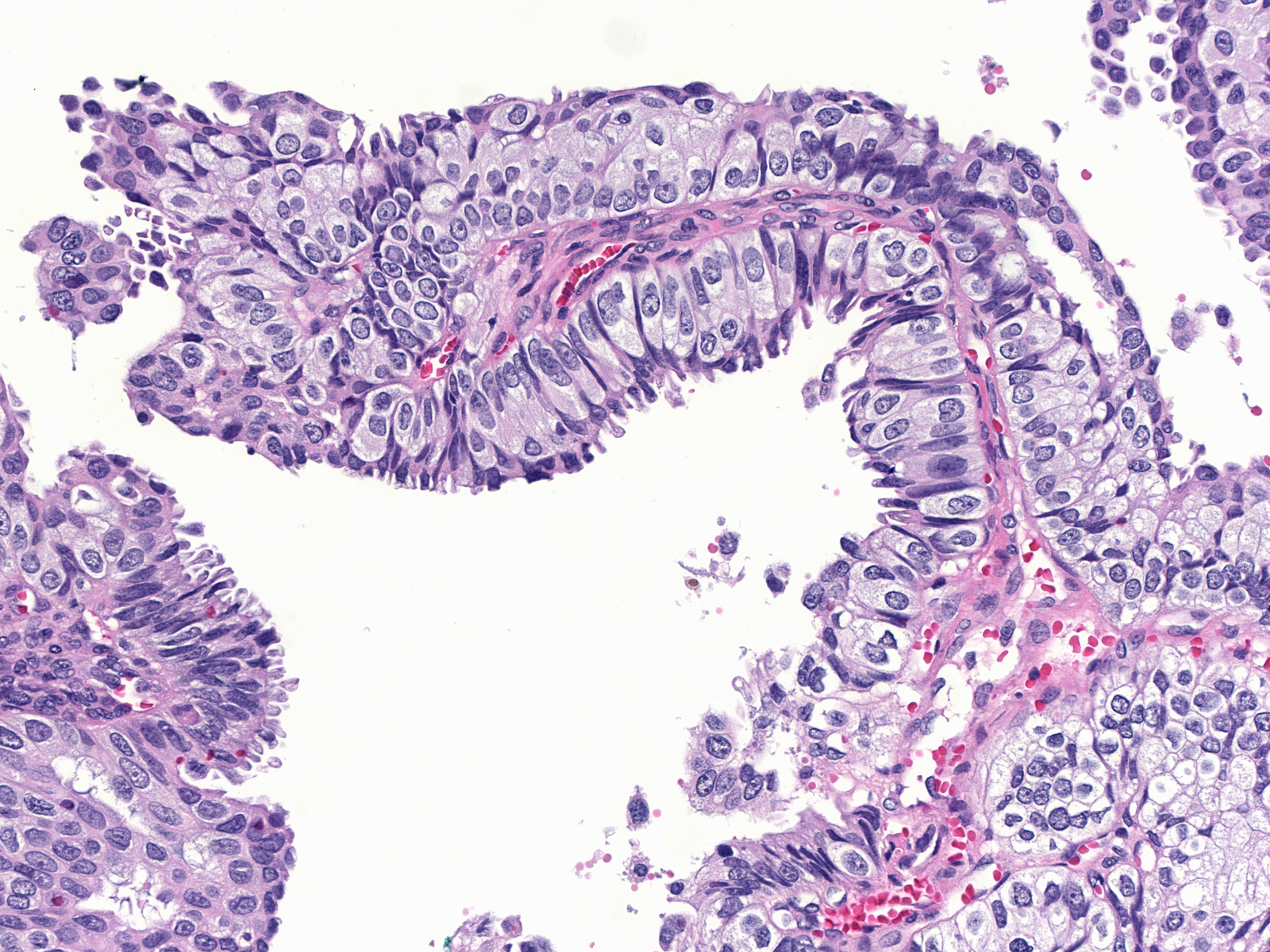
- Discussion: The papillary growth pattern distinguishes papillary carcinoma from all other mammary neoplasms except papilloma. Three morphological characteristics allow one to distinguish these two lesions.
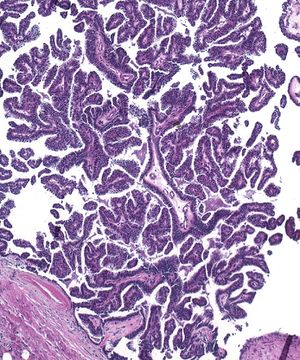
1. Papillary carcinomas consist of numerous irregular fronds of variable shape and dimension, which form a shaggy complex mass.
 |
 |
| Papillary carcinoma |
Papilloma |
This architecture contrasts with the structure of a papilloma, which consists of a few blunt fronds having geometric shapes and fitting together.
 |
 |
| Papillary carcinoma |
Papilloma |
2. The fronds of papillary carcinomas contain only scant fibrous connective tissue, whereas those of papillomas have substantial amounts of fibrous stroma.
 |
 |
| Papillary carcinoma |
Papilloma |
3. Malignant ductal cells constitute the entire neoplastic population of papillary carcinomas. In contrast, the epithelium of papillomas consists of luminal and myoepithelial cells both of which appear benign.
 |
 |
| Papillary carcinoma |
Papilloma |
Subtypes of Papillary Carcinoma
Papillary carcinomas usually exhibit both cystic and compact regions. When cystic growth predominates, the carcinoma looks like a shaggy nodule protruding into a large cavity filled with blood and debris. Pathologists use the term intracystic papillary carcinoma for papillary carcinomas with this macroscopic appearance. They apply the diagnosis of solid papillary carcinoma to those forming a compact mass. Solid papillary carcinomas typically display endocrine characteristics (Endocrine Carcinoma). Other varieties of papillary carcinoma include: encapsulated papillary carcinoma, in which a rind of reactive stroma encapsulates the tumor; dimorphic papillary carcinoma, in which the cells along the stromal cores possess pale or clear cytoplasm; and papillary carcinoma resembling tall cell variant of papillary thyroid carcinoma, in which the cells resemble those of a papillary thyroid carcinoma.
| This intracystic papillary carcinoma consists of a delicate, friable, shaggy nodule of tan tissue protruding into a cyst of several centimeters. The carcinoma cells form the cyst as well as the nodule. |
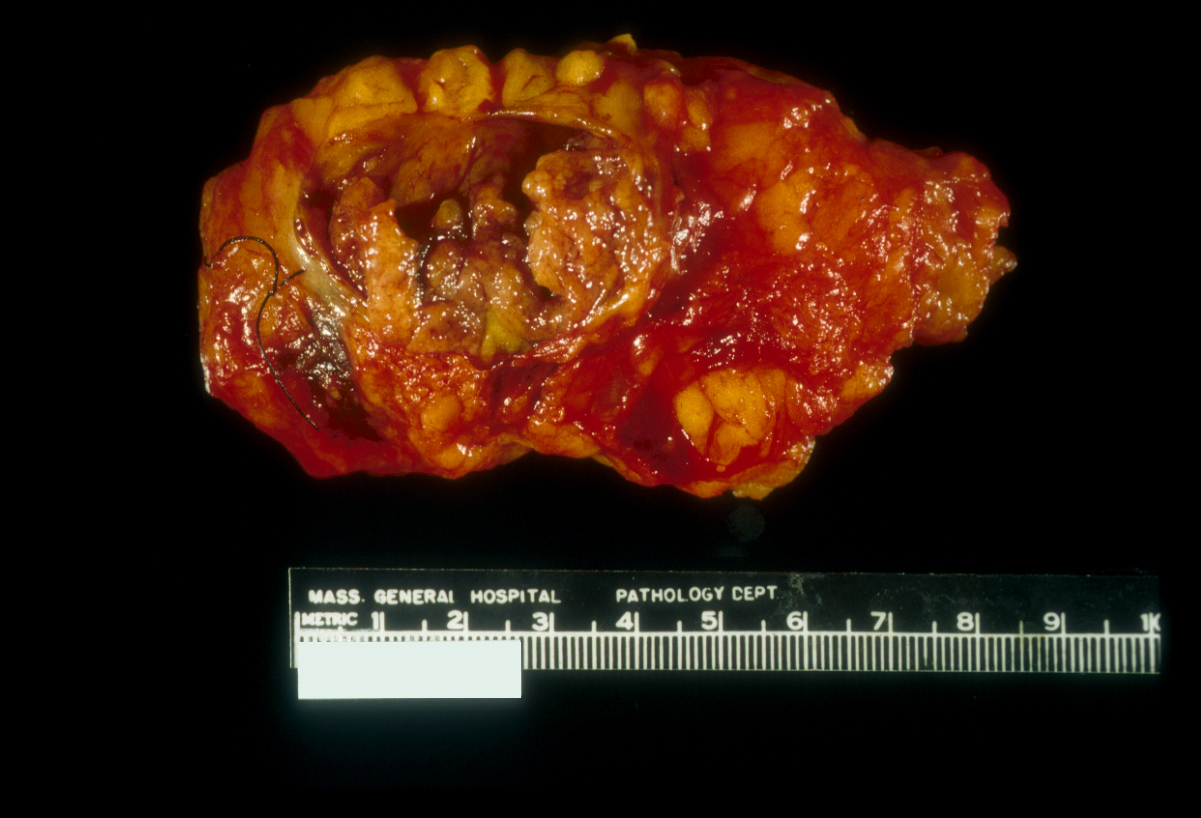 |
|
|
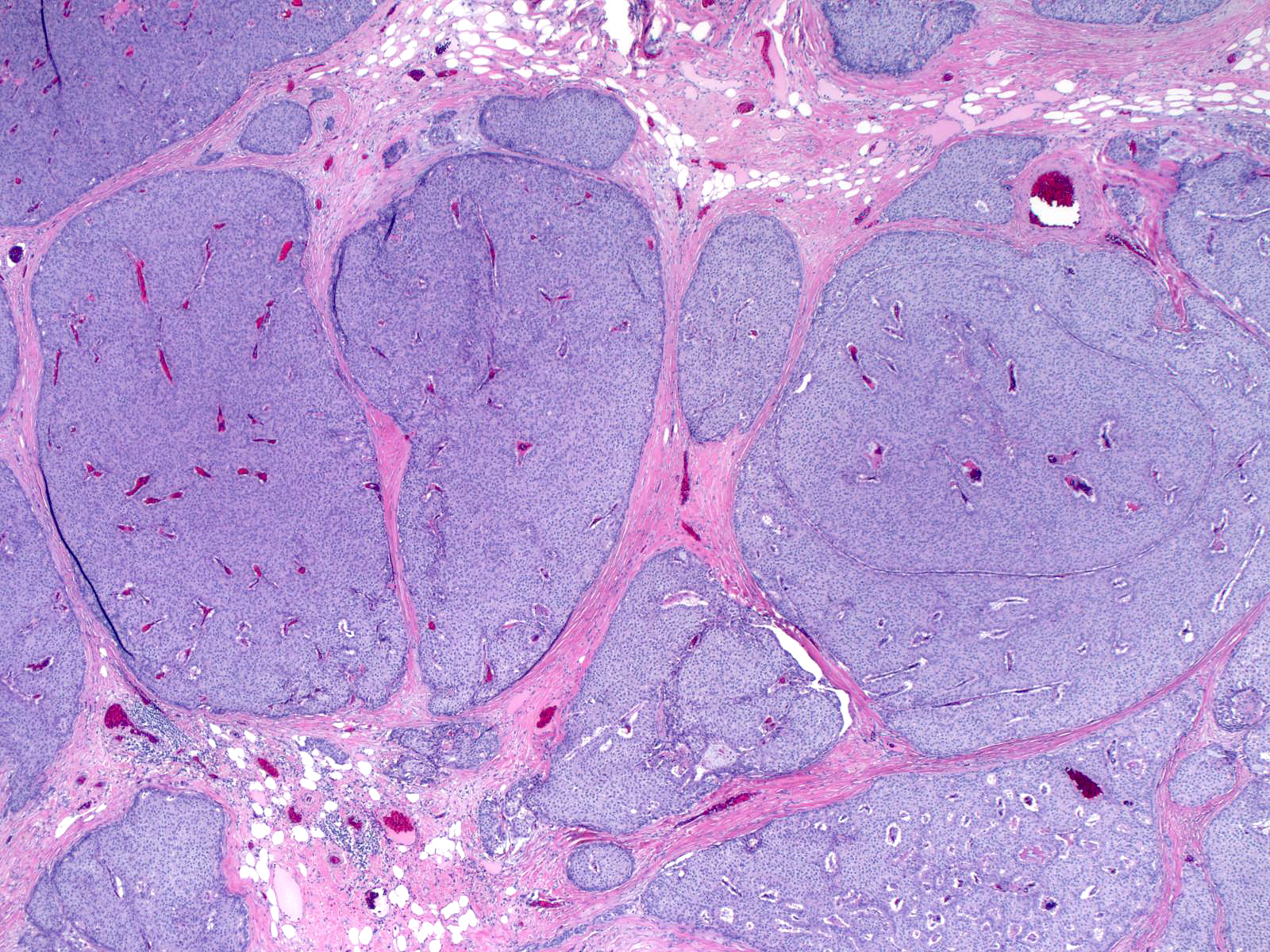
| Solid masses of carcinoma cells compose this solid papillary carcinoma. One cannot appreciate the underlying papillary architecture at this magnification, but the vascular skeletons within the nests hint at the papillary nature of the carcinoma. Solid papillary carcinomas typically display endocrine characteristics (Endocrine Carcinoma). |
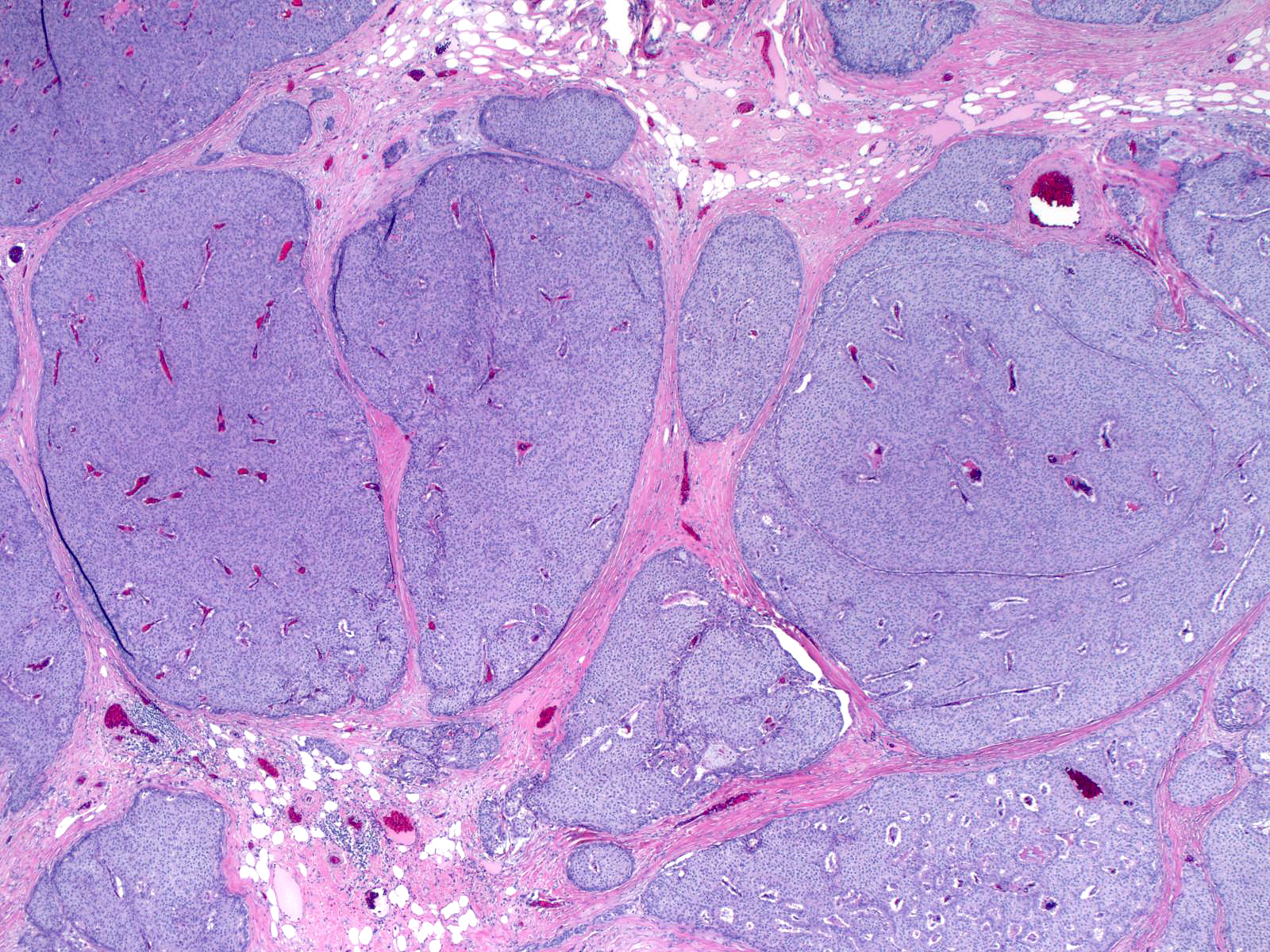 |
|
|
| A thick rim of reactive stroma surrounds this encapsulated papillary carcinoma. Some authors suggest that this subtype of papillary carcinoma has little metastatic potential. |
 |
|
|
| The basally positoned cells of a dimorphic papillary carcinoma have pale cytoplasm. One must not confuse them with myoepithelial cells. |
 |
|
|
| The columnar shape of the cells and the presence of colloid‑like secretions in papillary carcinoma resembling tall cell variant of thydoi carcinoma create a resemblance to this subtype of thyroid carcinoma. |
 |
|
|
Invasion of Papillary Carcinoma
Most conventional papillary carcinomas consist predominantly of invasive carcinoma, which typically forms round, partially cystic nests that mimic the appearance of intraductal growth. This phenomenon makes it difficult to recognize these collections as invasive, so one must always search for conclusive evidence of invasion when examining papillary carcinomas.
Such evidence of invasion consists of irregularities in the contour of the mass, fragmentation of the surrounding collagen bundles, and penetration of the stroma by small nests of carcinoma cells.
| Stains for myoepithelial cells will help to detect invasive collections. |
 |
|
|
Papilloma Overrun by Ductal Carcinoma In-Situ
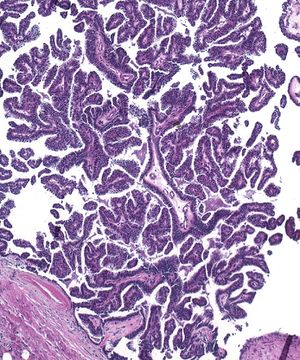
| Many noninvasive carcinomas with a papillary architecture represent papillomas overrun by ductal carcinoma in-situ. |
 |
|
|
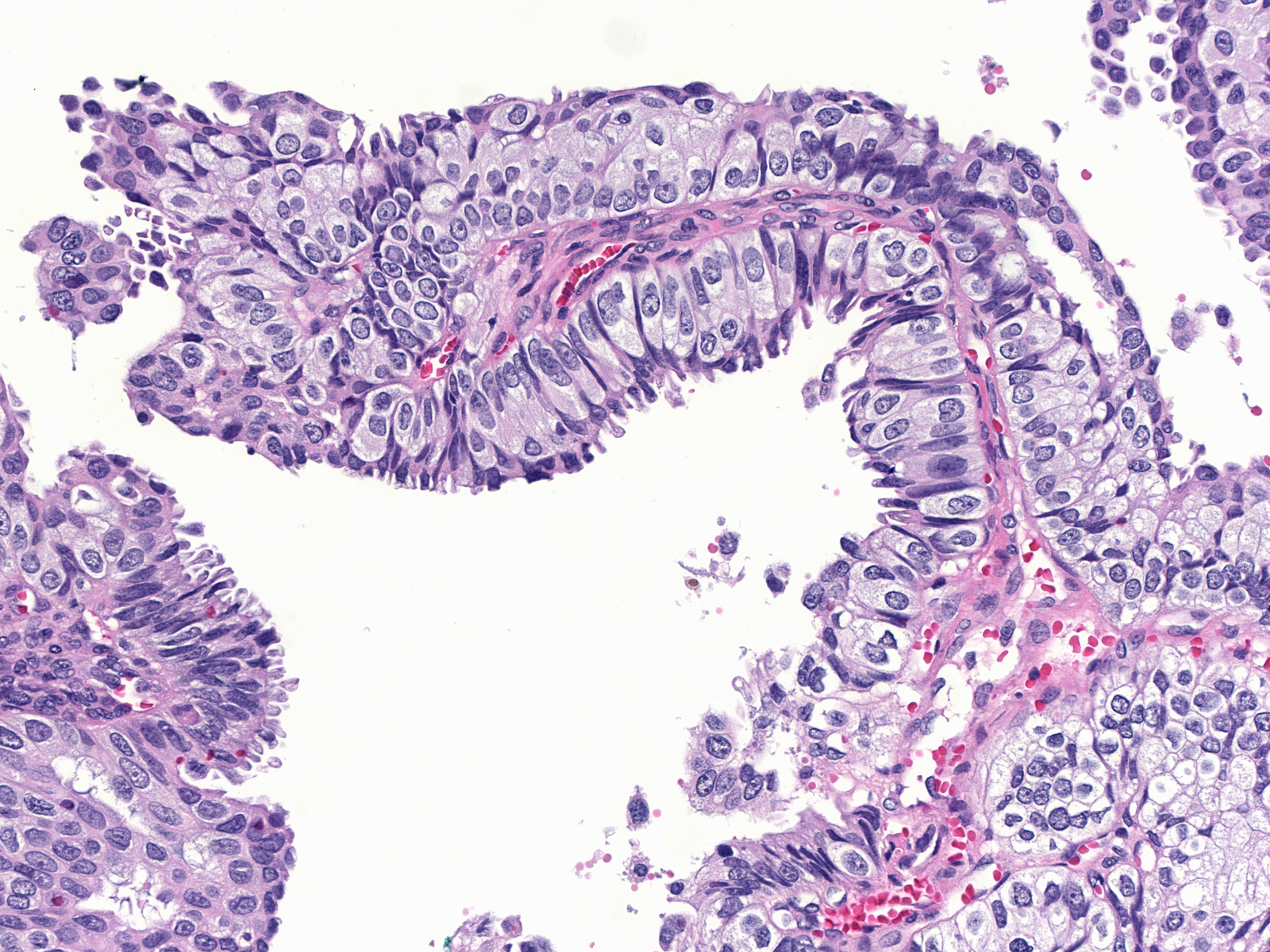
| To establish this diagnosis, one must find evidence of the pre-existing papilloma. The presence of benign epithelium, a substantial number of myoepithelial cells, or histiocytes in the stromal cores usually substantiates the notion of an underlying papilloma. The presence of ductal carcinoma in-situ in adjoining ducts would add additional but less substantial evidence to support the diagnosis of papilloma overrun by ductal carcinoma in-situ. |
 |
|
|
Breast Pathology