Difference between revisions of "Angiosarcoma"
| Line 33: | Line 33: | ||
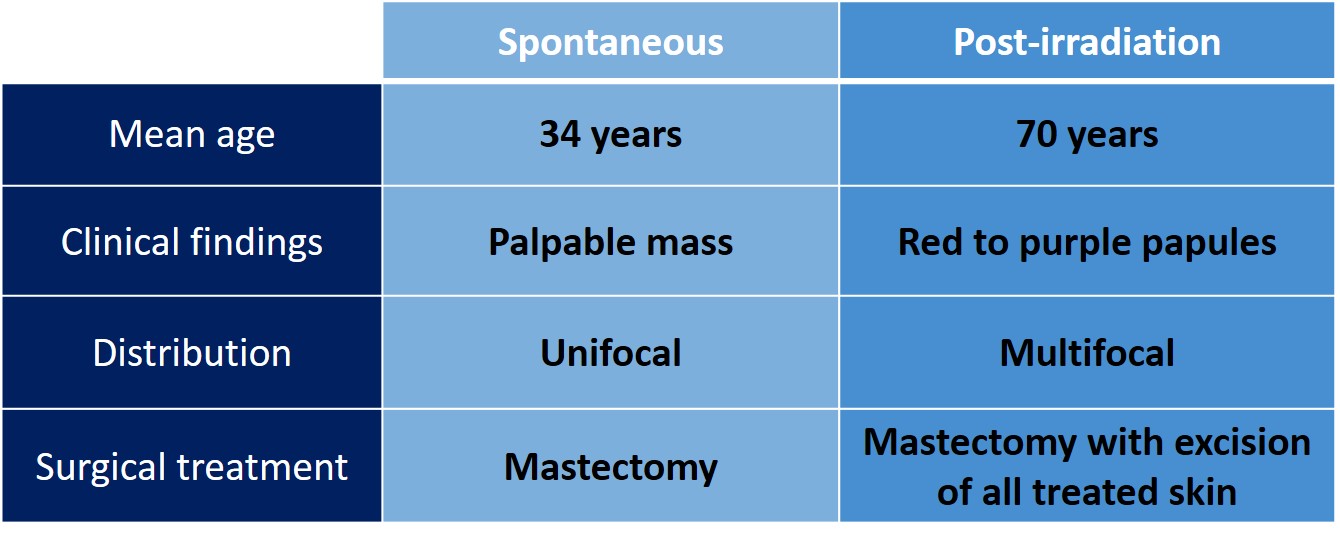
This table lists differences in the clinical findings of these two forms of angiosarcoma. | This table lists differences in the clinical findings of these two forms of angiosarcoma. | ||
{{img4|22-14 ASA_types_chart.jpg||}} | {{img4|22-14 ASA_types_chart.jpg||}} | ||
| + | tumor) can demonstrate this finding.|24-7 Beta_cat.jpg}} | ||
| + | == Quiz == | ||
| + | <bootstrap_collapse text="Start Quiz"><p><https://hub.partners.org/pathology/assessment/instructions?assessment_id=16535545" height="666" width="100%"></htmltag> | ||
| + | </p></bootstrap_collapse> | ||
Revision as of 16:54, July 13, 2020
General
- Definition: Angiosarcoma is a type of sarcoma comprise of neoplastic mesenchymal cells displaying characteristics of endothelial cells.
- Clinical Significance: Angiosarcomas arise either spontaneously or as a complication of breast irradiation. They present as a palpable mass in the breast; red, tan, or purple nodules in the skin; or abnormalities detected by radiological imaging. If a core biopsy discloses an angiosarcoma, a surgeon will usually carry out a mastectomy. Angiosarcomas spread to axillary lymph nodes so rarely that surgeons do not remove them unless they seem suspicious by physical or radiological examination.
- Gross Findings: The tumors appear tan to red and feel fleshy. Almost all spontaneous angiosarcomas span more than three centimeters.
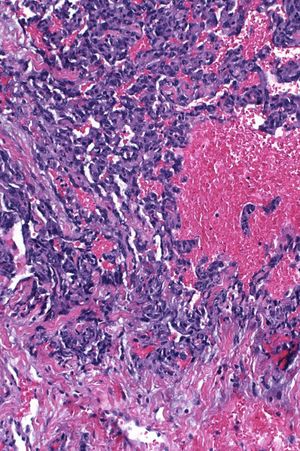
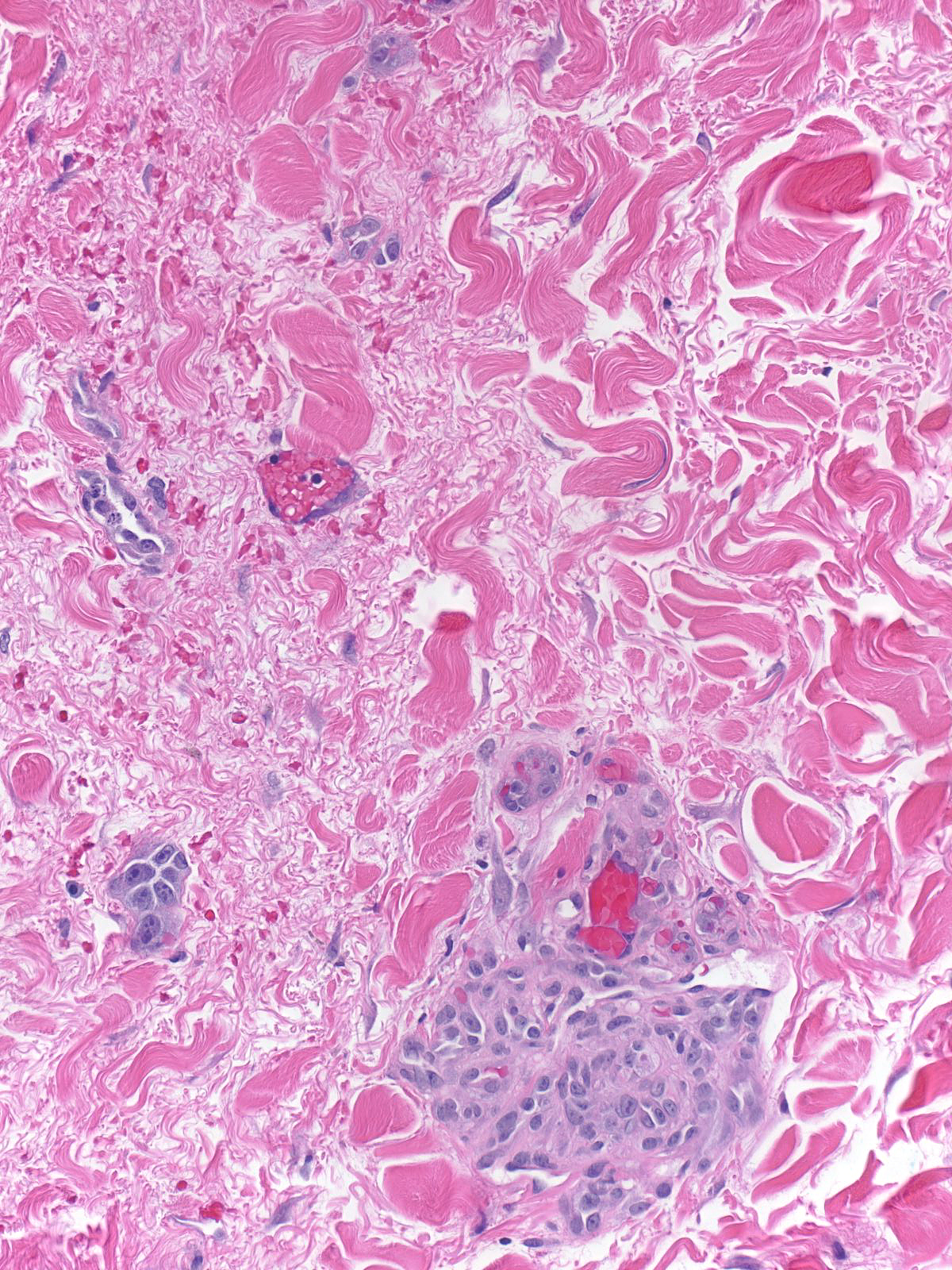
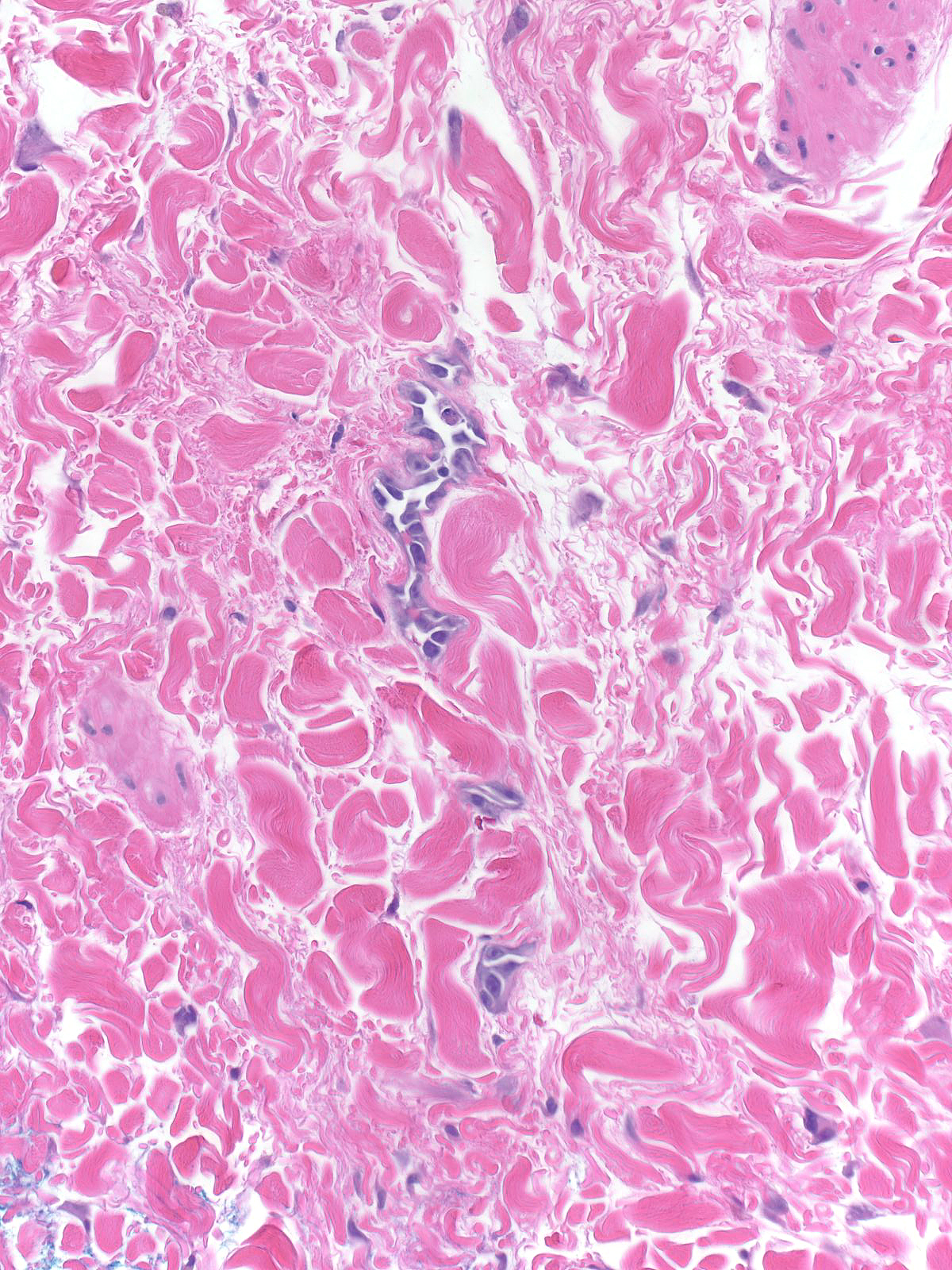
- Microscopic Findings: Angiosarcomas of the breast exhibit the microscopic features shown by angiosarcomas arising in other organs.
- Differential Diagnosis: Hemangioma (less than three centimeters, no atypia), other sarcomas (no endothelial differentiation), high‑grade invasive ductal carcinoma (epithelial proteins), angiolipoma (noninfiltrative borders), and atypical vascular lesion (no atypia, classic shape and location, c-myc negative) (Atypical vascular lesions are benign proliferations of either lymphatic vessels or blood vessels that arise in the dermis several years following the completion of breast irradiation. They do not ordinarily evolve into angiosarcomas.)
- Discussion: Most mammary angiosarcomas exhibit vasoformative areas, but the extent of vessel formation depends on the grade of the sarcoma. The malignant cells stain for proteins found in endothelial cells. In certain cases, the neoplastic cells stain for D2‑40, but this reactivity is not universal. High‑grade epithelioid angiosarcomas can stain for keratin.
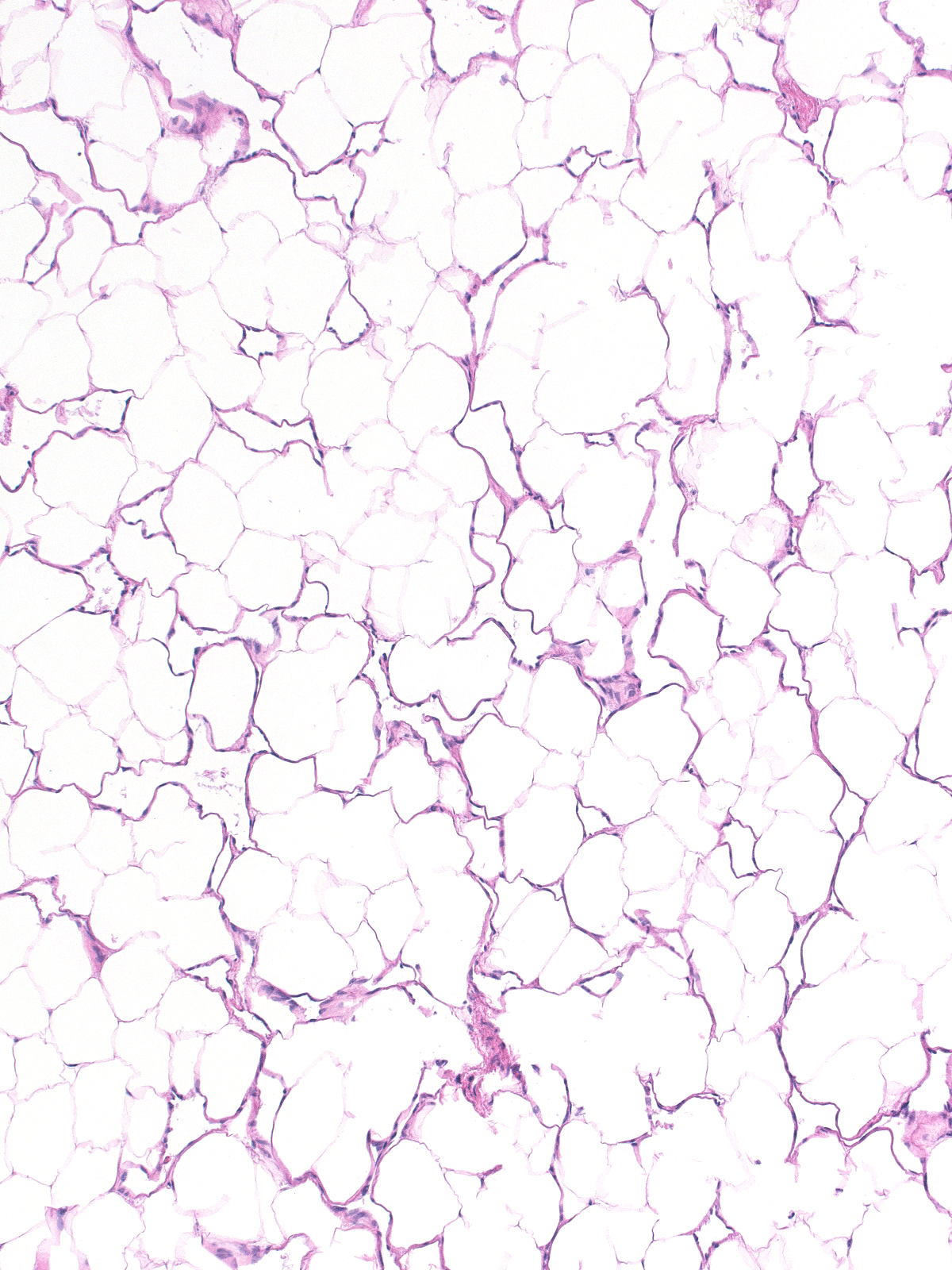
Low-grade examples display clearly formed blood vessels, whereas high-grade angiosarcomas consist of cellular masses showing limited formation of vessels.
 |
 |
| A single layer of flat, bland, neoplastic endothelial cells lines the vessels in low-grade angiosarcomas. | 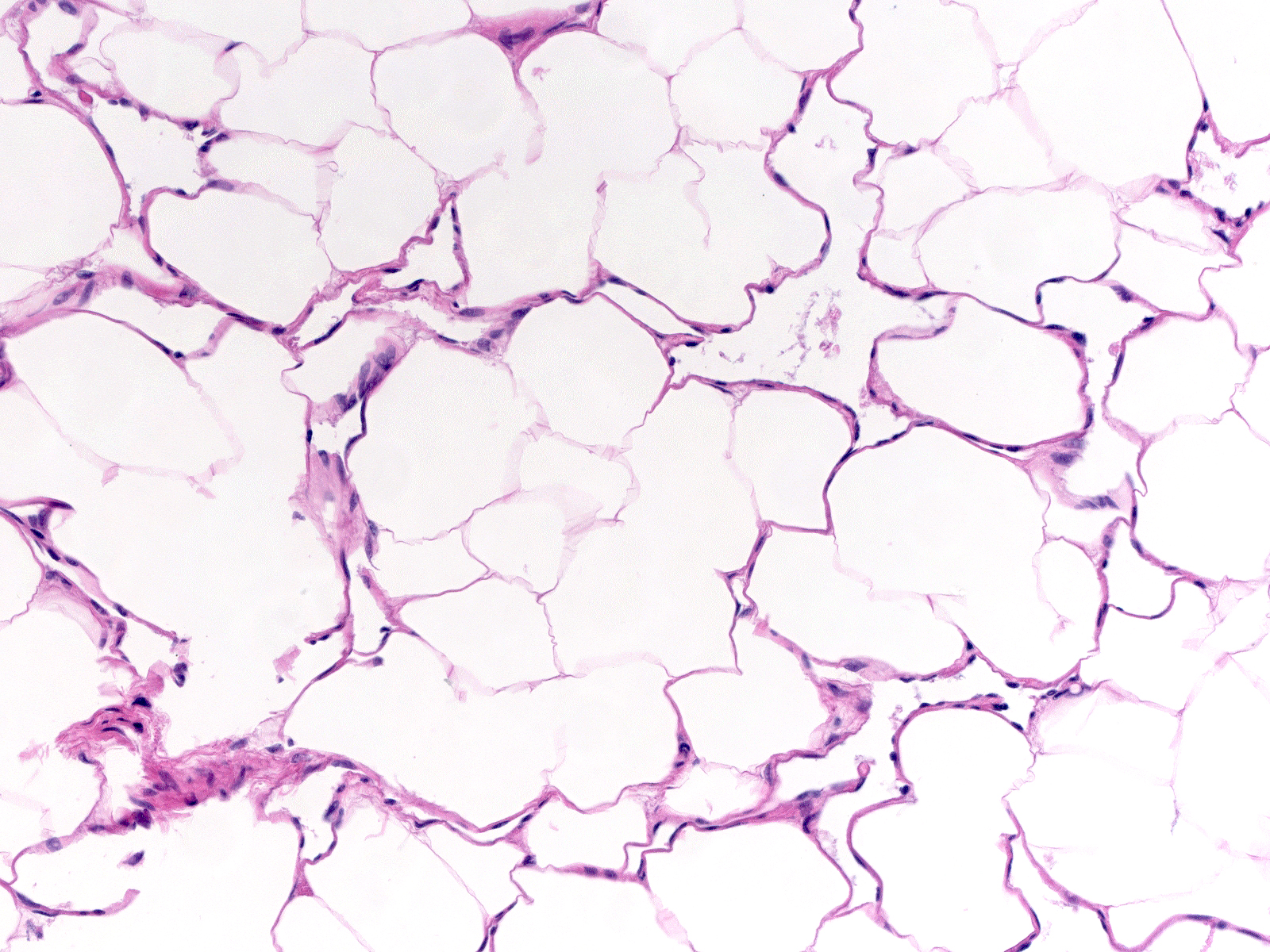 |
| The neoplastic vascular cells in high-grade tumors pile up and create endothelial tufts and micropapillae. | 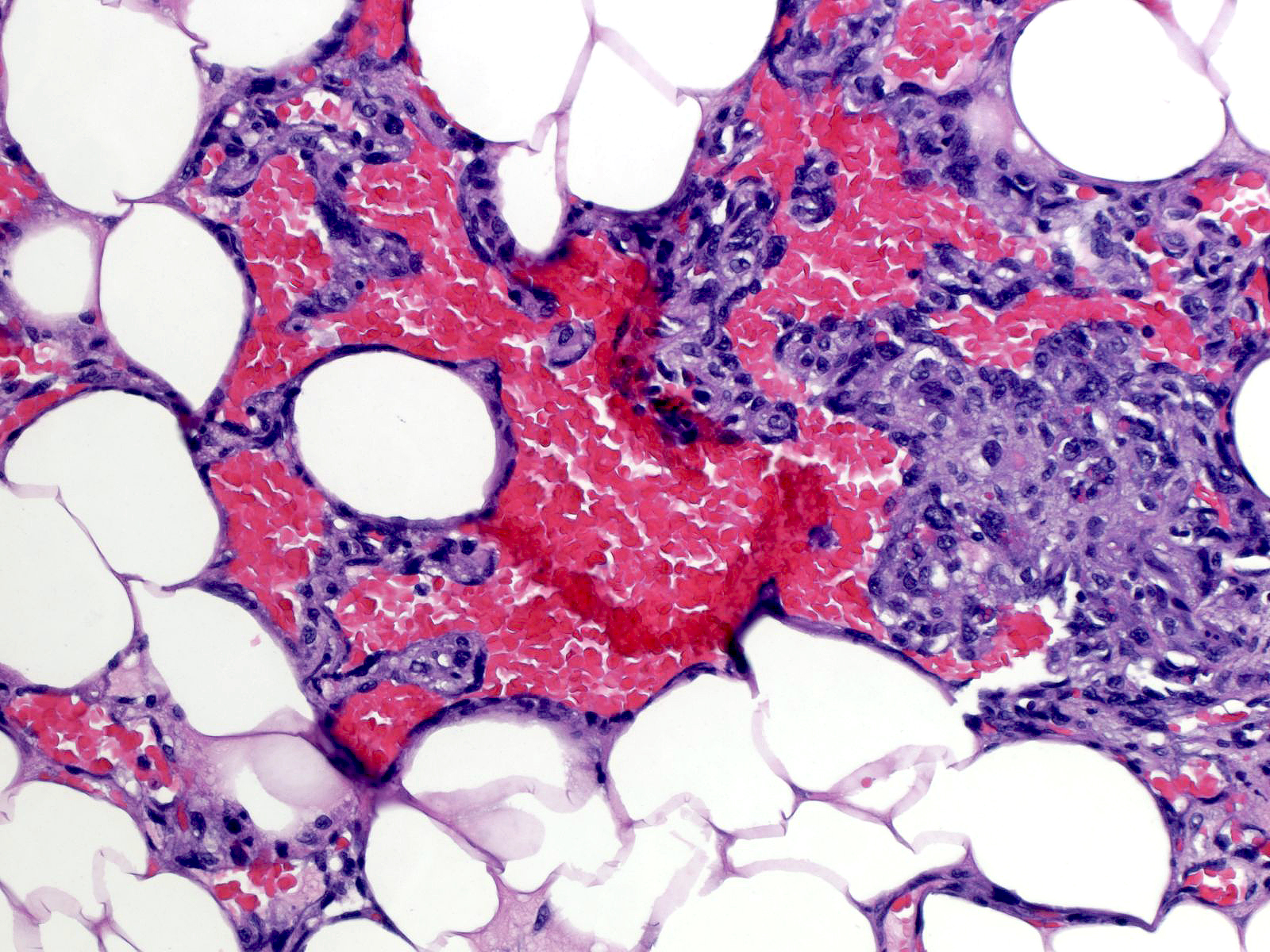 |
| The cells in solid foci have spindled to oval shapes; they sometimes look epithelioid. | 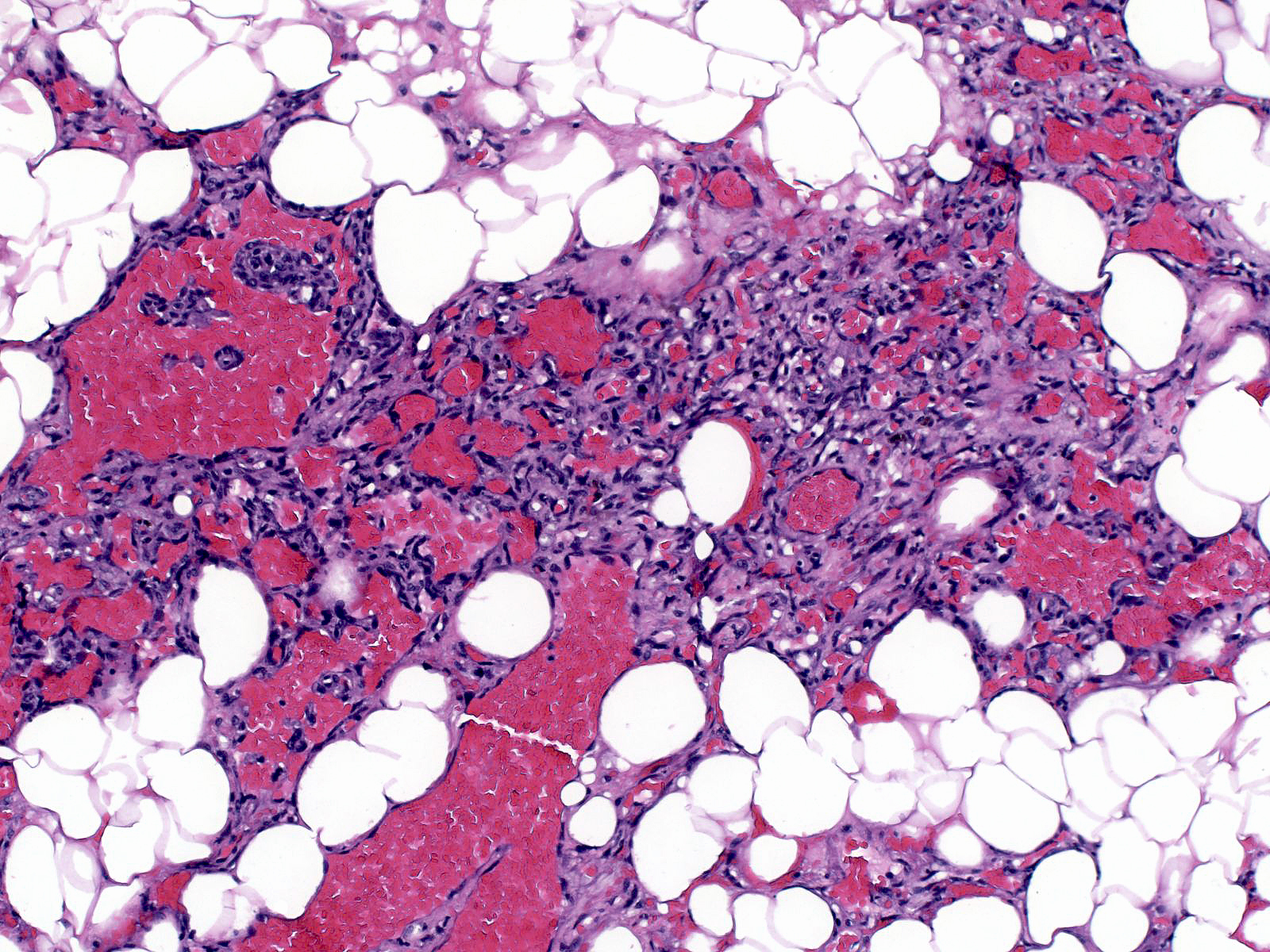 |
| The neoplastic cells possess hyperchromatic, pleomorphic nuclei. | 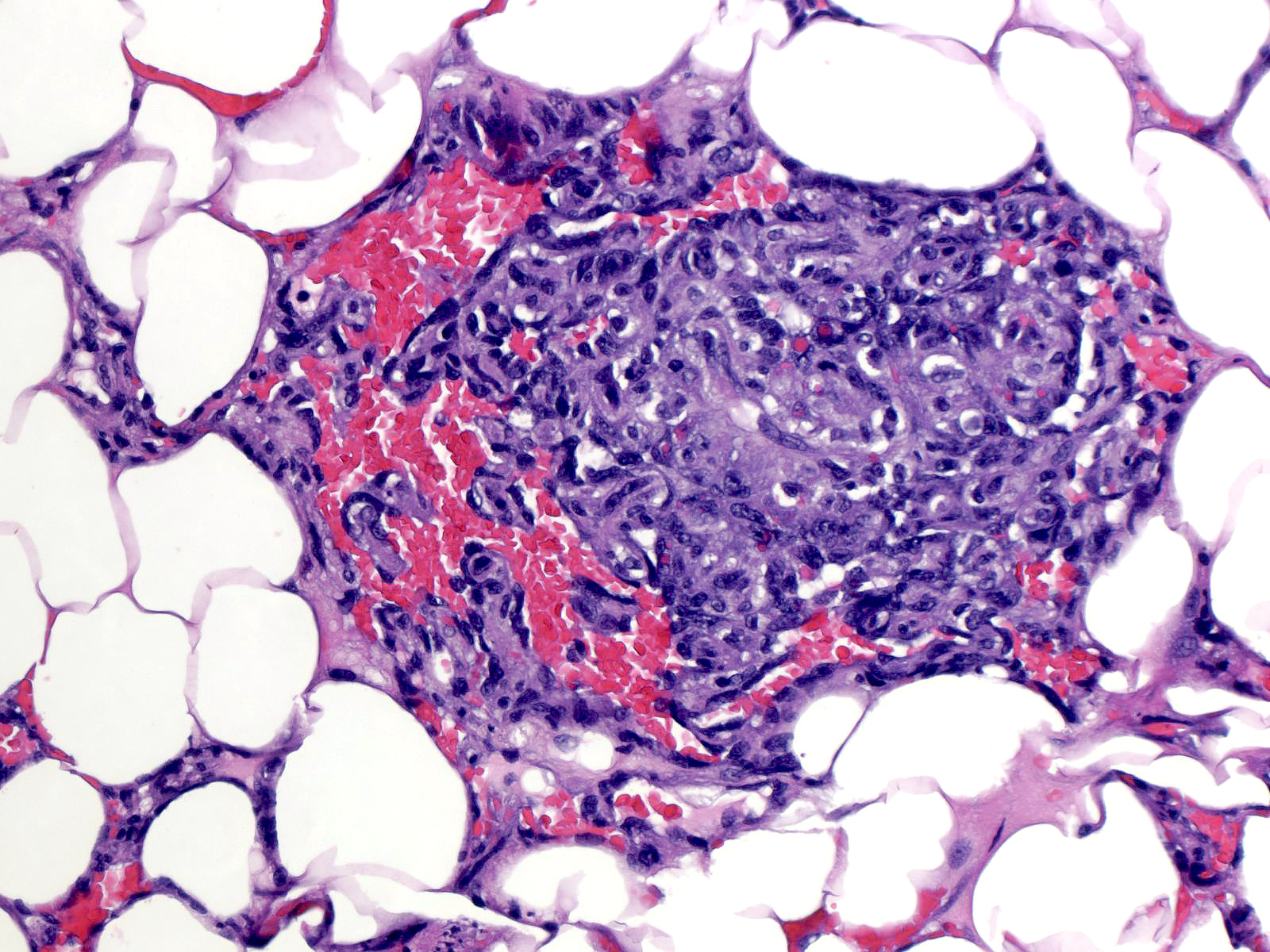 |
| In high-grade tumors, mitotic figures are plentiful, especially in regions of solid growth. | 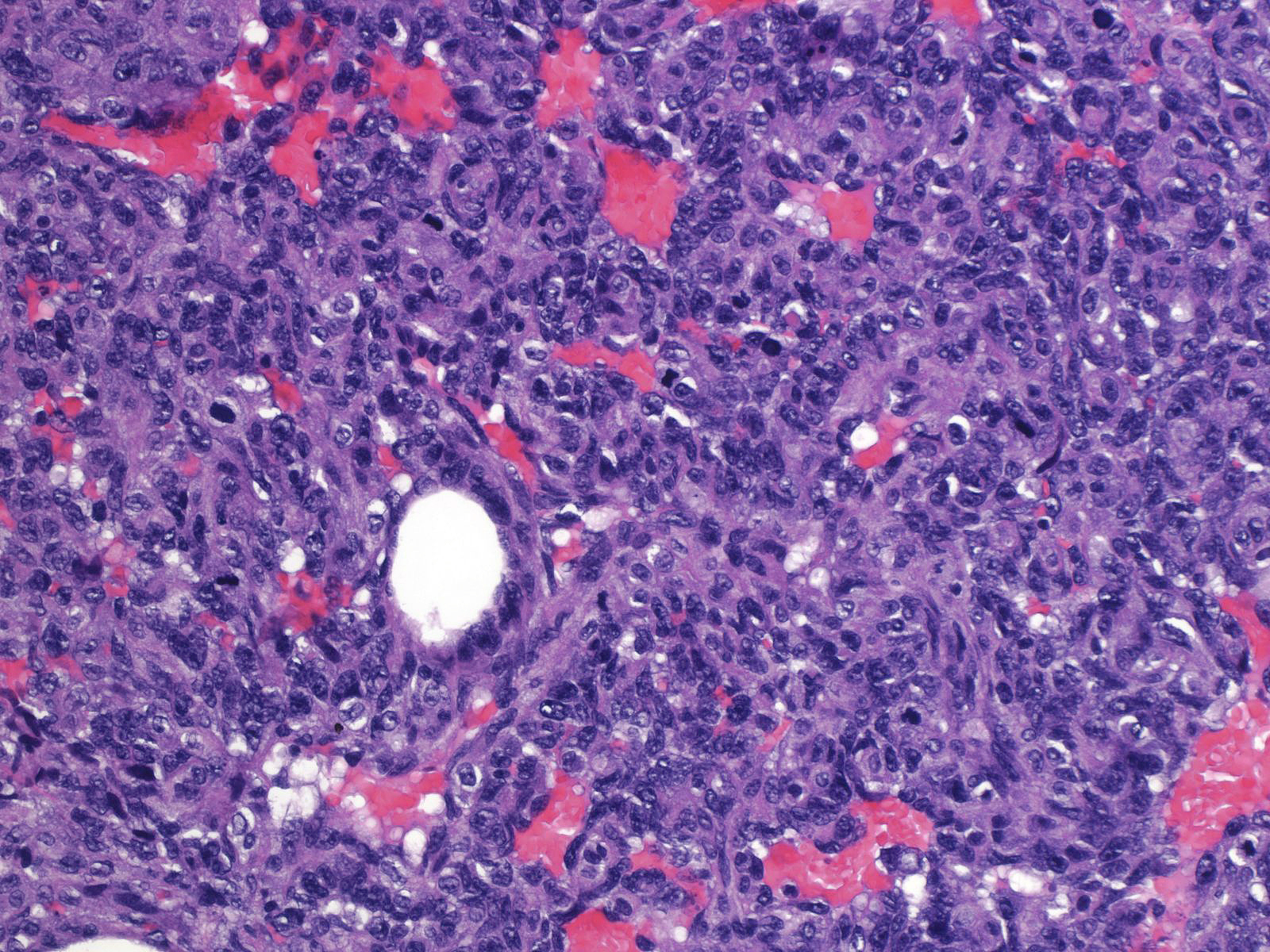 |
| Extravasated erythrocytes can collect in large numbers to form a blood lake. Blood lakes often arise in regions of necrosis. Only high‑grade angiosarcomas contain blood lakes. | 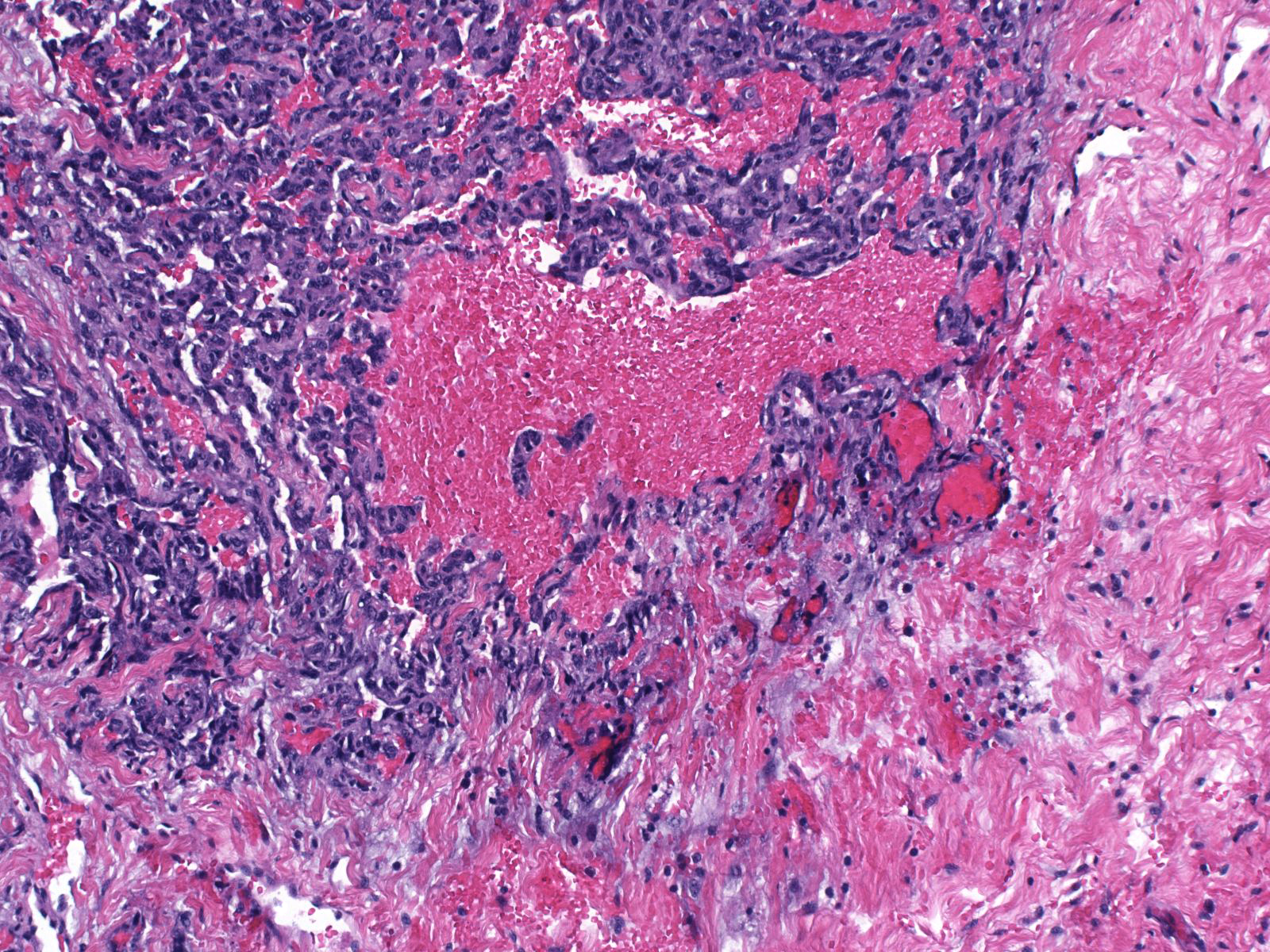 |
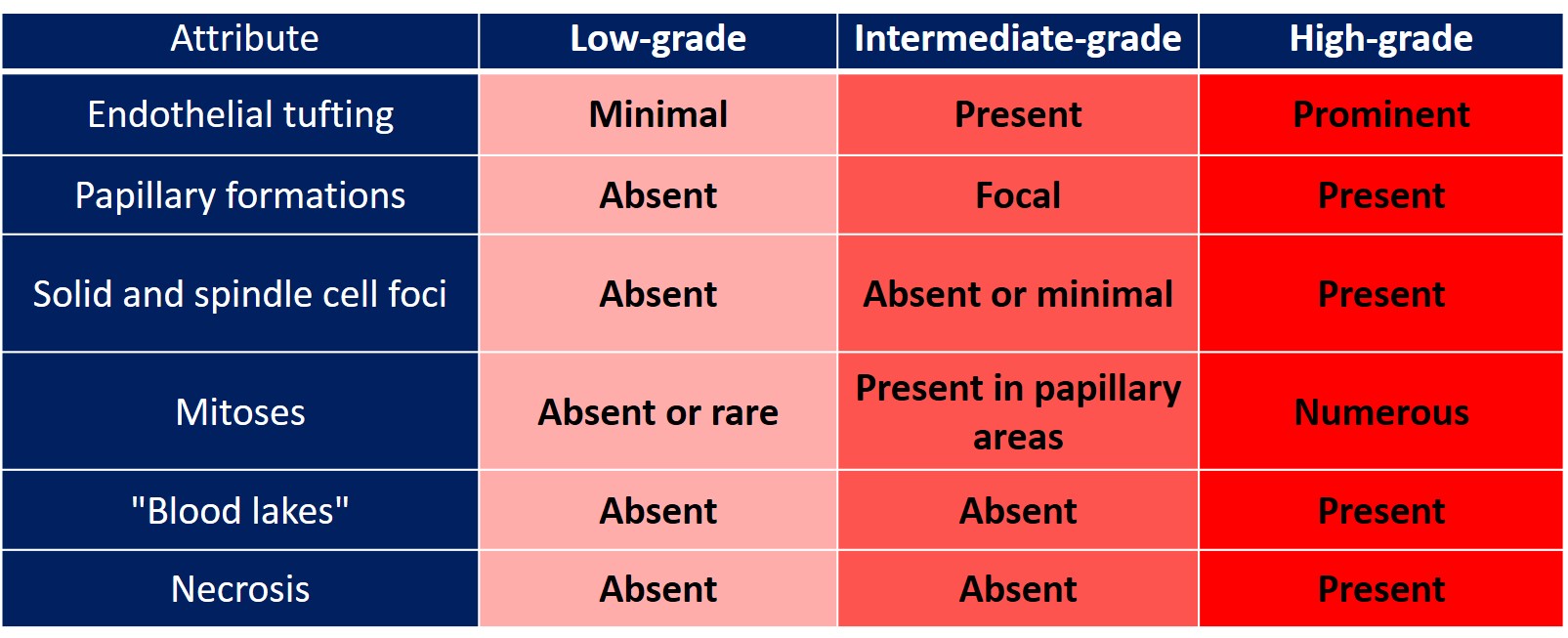
This chart lists features used when grading mammary angiosarcomas.
 |
|
Sporadic and post‑irradiation angiosarcomas share many features, but the sarcomas arising in these two situations differ in several ways. First post‑irradiation angiosarcomas usually arise in the skin and in seemingly independent foci. Second, post‑irradiation angiosarcomas typically grow as dispersed small clusters infiltrating the dermis rather than forming a compact mass in the way that spontaneous angiosarcomas do. Third, post‑irradiation angiosarcomas stain for c‑myc, whereas spontaneous angiosarcomas do not.
Post-irradiation angiosarcoma infiltrates the dermis.
 |
 |
A stain for c-Myc
 |
|
This table lists differences in the clinical findings of these two forms of angiosarcoma.
 |
|
tumor) can demonstrate this finding.|24-7 Beta_cat.jpg}}
Quiz
<https://hub.partners.org/pathology/assessment/instructions?assessment_id=16535545" height="666" width="100%"></htmltag>