Difference between revisions of "mgh:breast-Basic Gross Pathology"
| (One intermediate revision by one other user not shown) | |||
| Line 2: | Line 2: | ||
{{:TOC}} | {{:TOC}} | ||
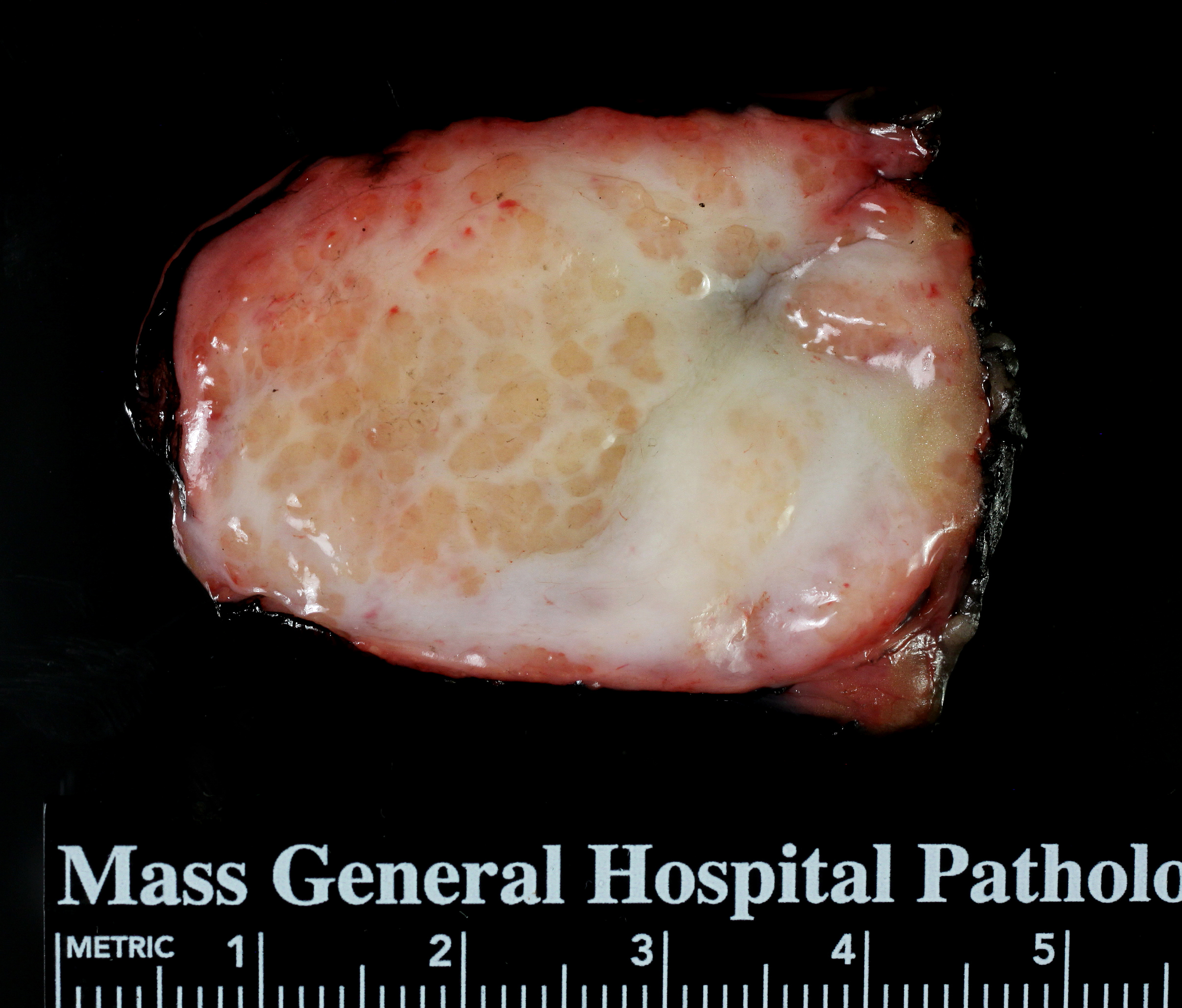
== Normal Tissue == | == Normal Tissue == | ||
| − | {{ | + | {{img3|2-1 BG normal-hp 6.30.14.jpeg-2.jpeg|2-2 BG Fibrous-breast-hp 6.30.14.jpeg.jpg|2-3 Fatty Breast 7.23.14 hp-2.jpeg|Normal - The parenchyma consists of glandular tissue, fibrous connective tissue, and fat.|Fibrous Breast - Fibrous tissue predominates over fat in the breasts of young women.|Fatty Breast - Fat is the dominate component of older breast parenchyma.|}} |
Mammary parenchyma consists of glandular tissue, fibrous connective tissue, and fat. In most circumstances, one cannot usually discern the glandular tissue by eye; however, during pregnancy, enlargement of the lobules causes them to appear as tan nodules a millimeter or so in diameter. The fibrous connective tissue consists of firm, dense, white bands of tissue, which extend into the surrounding yellow, adipose tissue. The proportions of fibrous tissue and fat vary from patient to patient and according to the age of the patient. The breasts of young women usually contain more fibrous tissue than fat, whereas fat dominates in the breasts of older women. The subareolar and central regions typically contain more fibrous tissue than the peripheral zones. An inexperienced observer can mistake the normal, abundant fibrous tissue beneath the nipple as a carcinoma -- avoid this mistake. | Mammary parenchyma consists of glandular tissue, fibrous connective tissue, and fat. In most circumstances, one cannot usually discern the glandular tissue by eye; however, during pregnancy, enlargement of the lobules causes them to appear as tan nodules a millimeter or so in diameter. The fibrous connective tissue consists of firm, dense, white bands of tissue, which extend into the surrounding yellow, adipose tissue. The proportions of fibrous tissue and fat vary from patient to patient and according to the age of the patient. The breasts of young women usually contain more fibrous tissue than fat, whereas fat dominates in the breasts of older women. The subareolar and central regions typically contain more fibrous tissue than the peripheral zones. An inexperienced observer can mistake the normal, abundant fibrous tissue beneath the nipple as a carcinoma -- avoid this mistake. | ||
== Iatrogenic Changes == | == Iatrogenic Changes == | ||
| Line 27: | Line 27: | ||
Systemic treatment, most commonly cytotoxic chemotherapy, often alters the appearance of carcinomas. If the carcinoma disappears completely, one sees an poorly defined, irregular region of rubbery tissue with a characteristic pink grey and pale yellow hue. Pathologists refer to such a region as the tumor bed. | Systemic treatment, most commonly cytotoxic chemotherapy, often alters the appearance of carcinomas. If the carcinoma disappears completely, one sees an poorly defined, irregular region of rubbery tissue with a characteristic pink grey and pale yellow hue. Pathologists refer to such a region as the tumor bed. | ||
{{img1|Carcinoma after neoadjuvant therapy (tumor bed)|2-27 BG_Neoadjuvant_6.23.14.jpg|}} | {{img1|Carcinoma after neoadjuvant therapy (tumor bed)|2-27 BG_Neoadjuvant_6.23.14.jpg|}} | ||
| − | + | {{:mgh:breast-footer}} | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Latest revision as of 09:39, July 14, 2020
Contents
Normal Tissue
 |
 |
 |
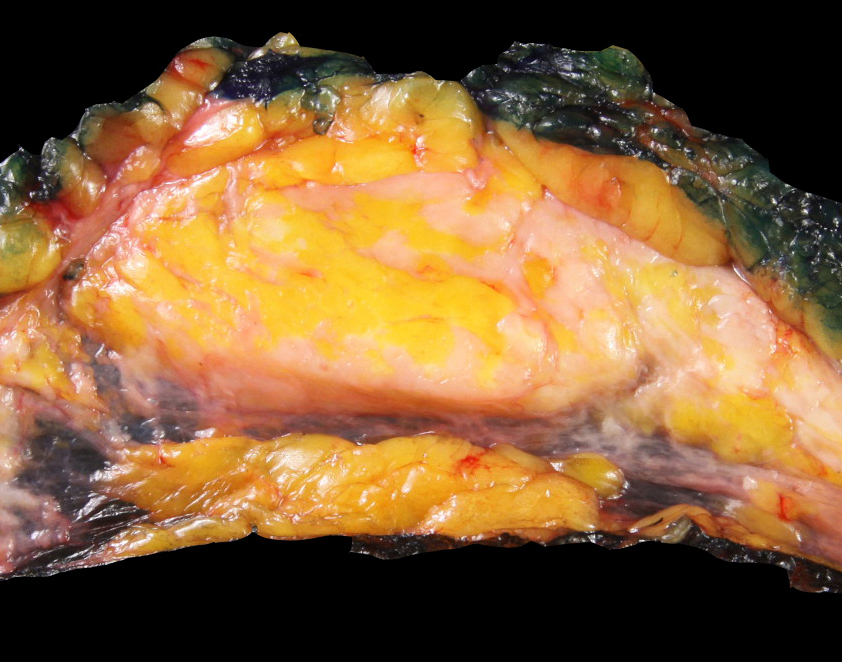
Mammary parenchyma consists of glandular tissue, fibrous connective tissue, and fat. In most circumstances, one cannot usually discern the glandular tissue by eye; however, during pregnancy, enlargement of the lobules causes them to appear as tan nodules a millimeter or so in diameter. The fibrous connective tissue consists of firm, dense, white bands of tissue, which extend into the surrounding yellow, adipose tissue. The proportions of fibrous tissue and fat vary from patient to patient and according to the age of the patient. The breasts of young women usually contain more fibrous tissue than fat, whereas fat dominates in the breasts of older women. The subareolar and central regions typically contain more fibrous tissue than the peripheral zones. An inexperienced observer can mistake the normal, abundant fibrous tissue beneath the nipple as a carcinoma -- avoid this mistake.
Iatrogenic Changes
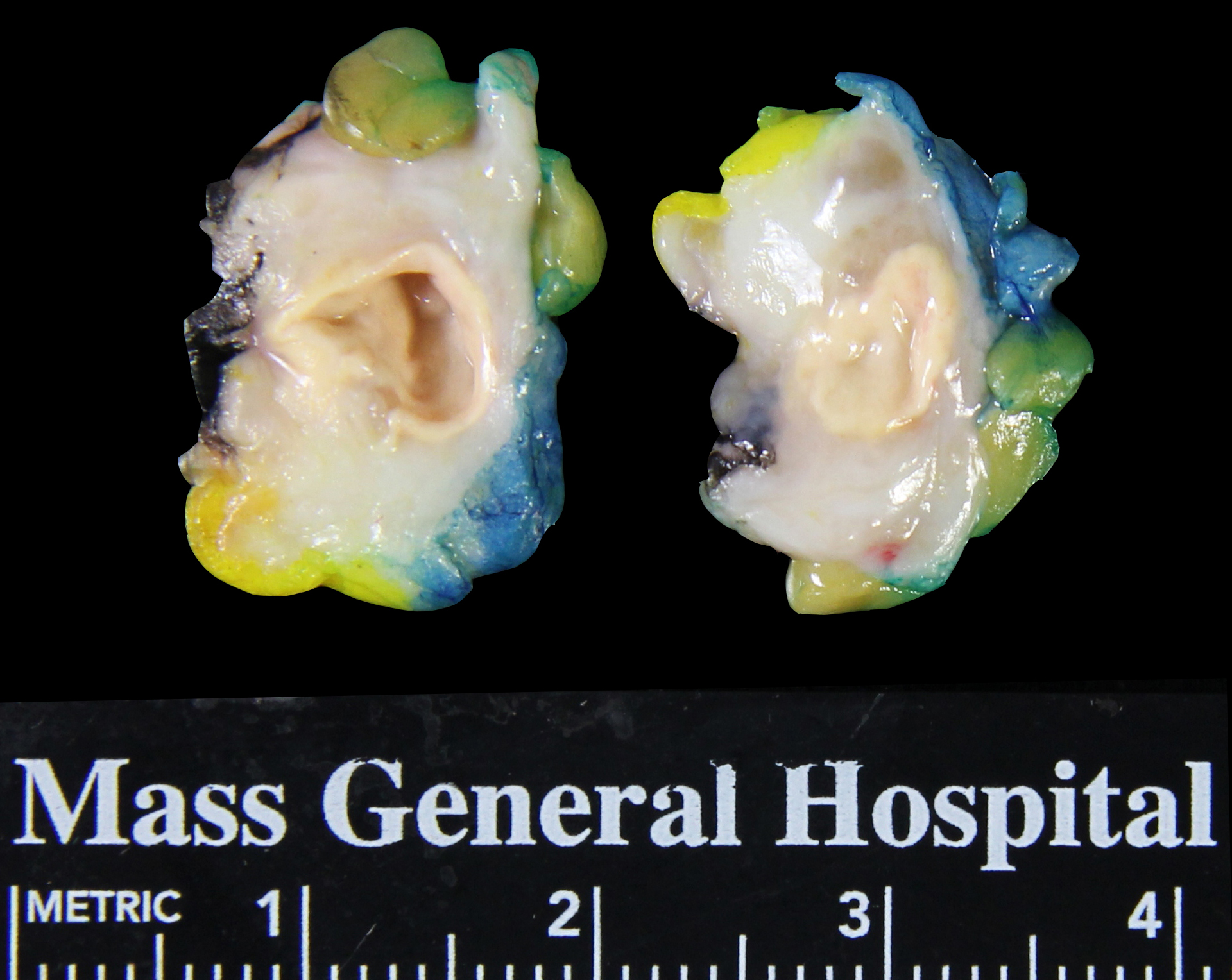
| Methylene blue: Surgeons inject this blue dye into the breast during sentinel node mapping. The presence of the blue color does not indicate a pathological process. (Breast tissue discolored by methylene blue) | 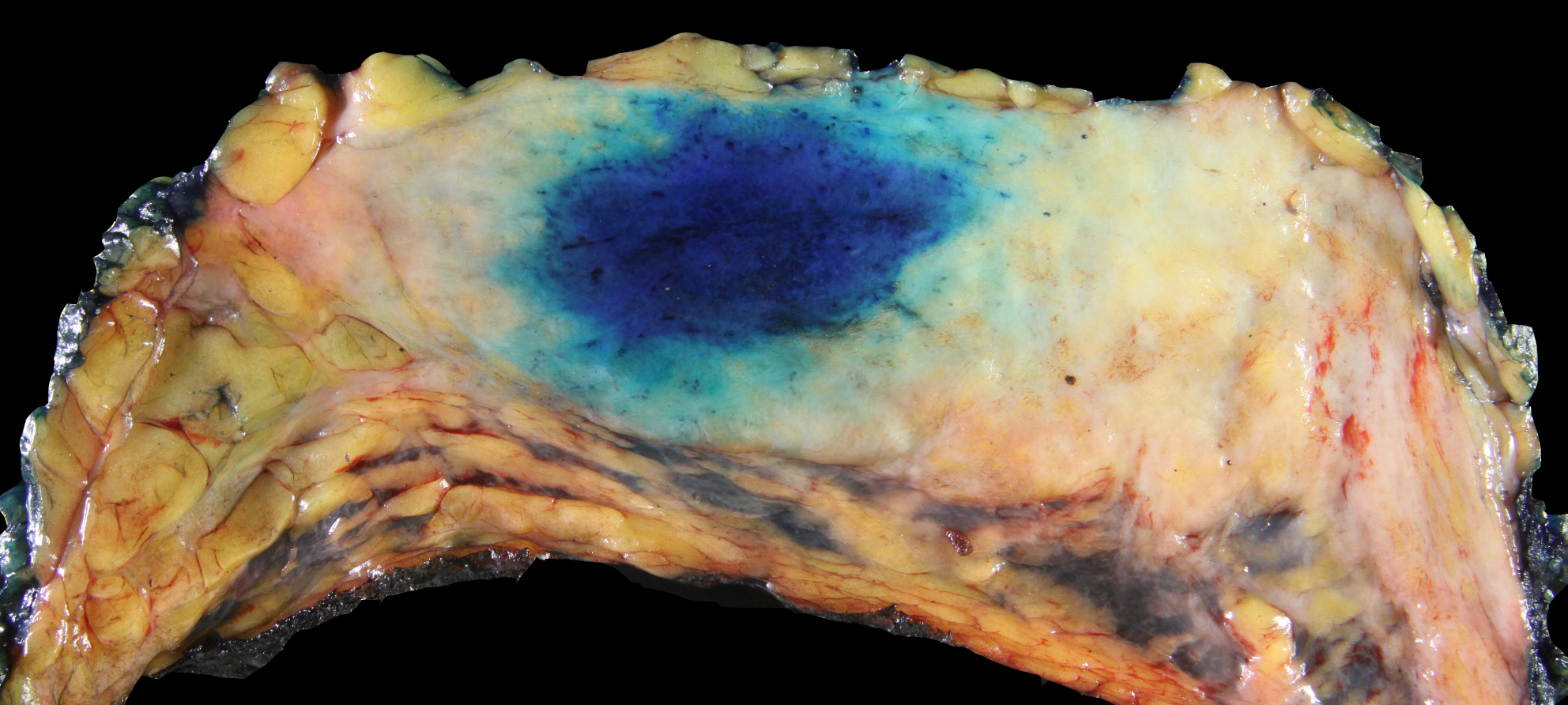 |
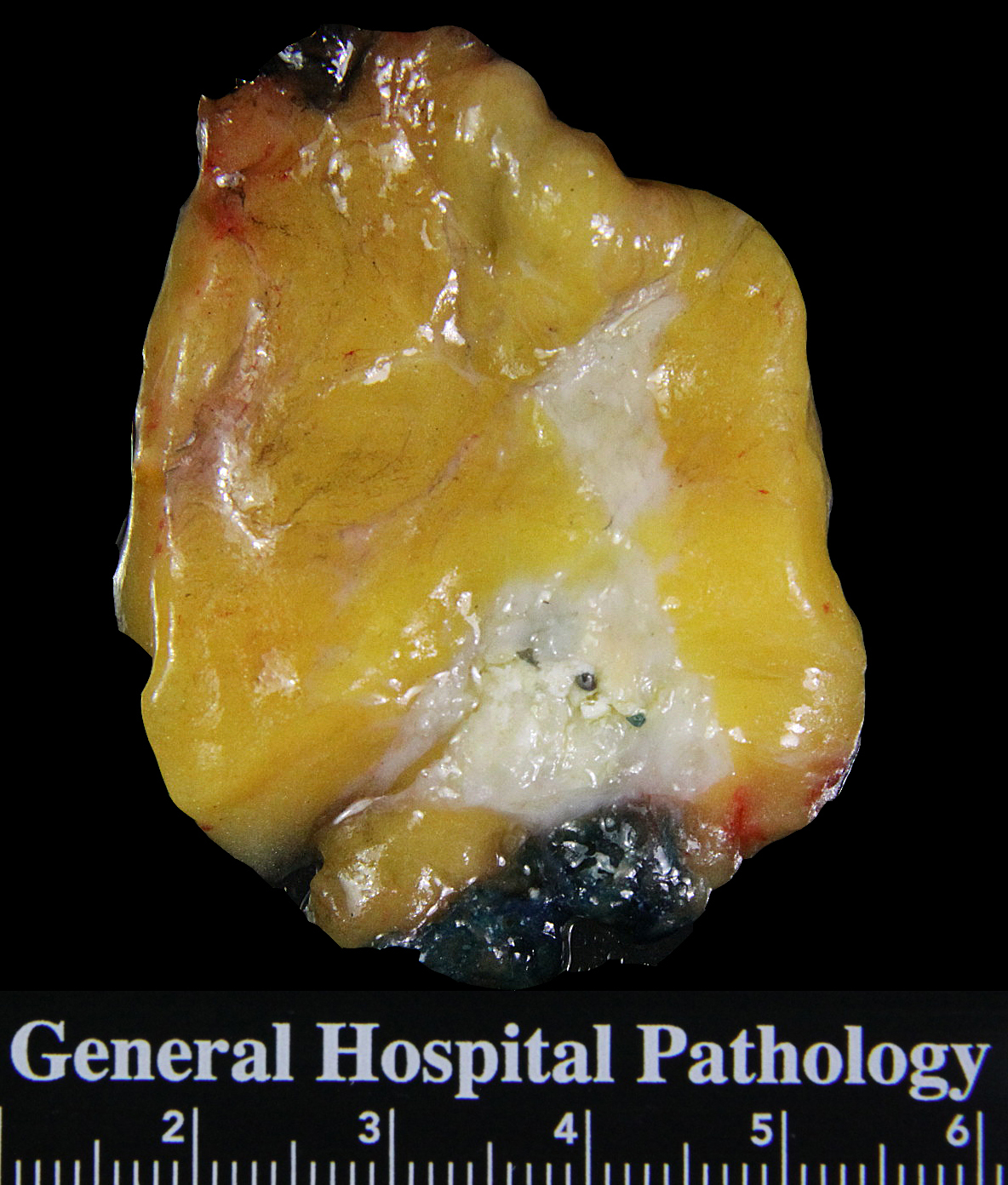
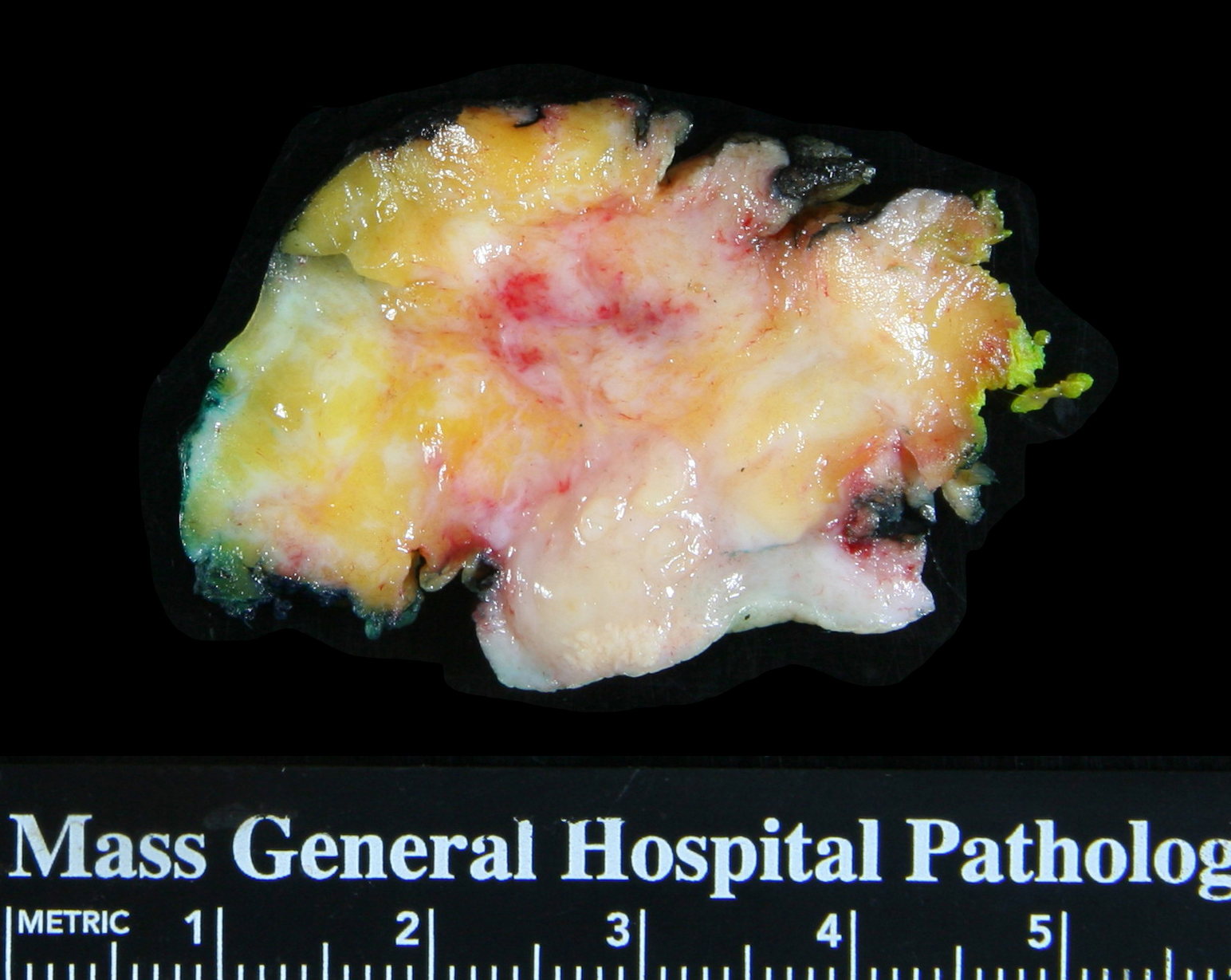
Core biopsy alterations: Needle core biopsy sites change with the progression of healing. The altered area usually spans less than one centimeter and often measures only a few millimeters. During the first two weeks, a well defined, approximately round, rubbery region of mottled, yellow‑white, tan, or red tissue marks the site of the biopsy. Fat necrosis accounts for the yellow‑white color. Foci of fat necrosis often contain small, white deposits commonly described as chalky. Hemorrhage caused by the biopsy explains the red hue. Healing leads to the formation of an ill defined, spiculated, rubbery, mottled tan and white mass that extends into the surrounding parenchyma. Excess bleeding results in a hematoma, which usually delays healing. Radiologists outside MGH sometimes inject foreign material (commonly denatured bovine collagen) at the site of a core biopsy to promote coagulation, and one may see this pale, granular, friable substance within the altered tissue. After several months, it becomes impossible to identify the biopsy site.
 |
 |
 |
 |
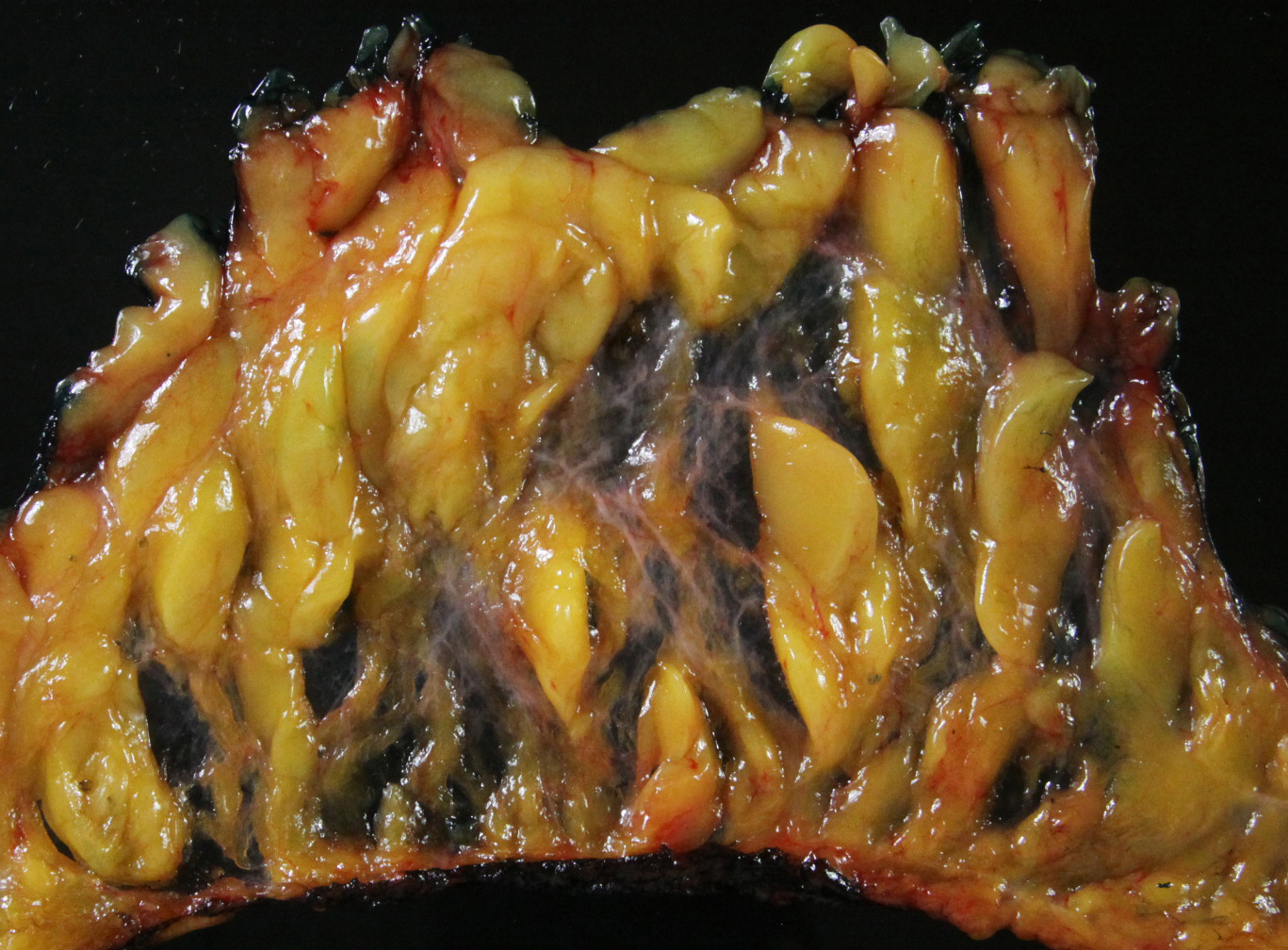
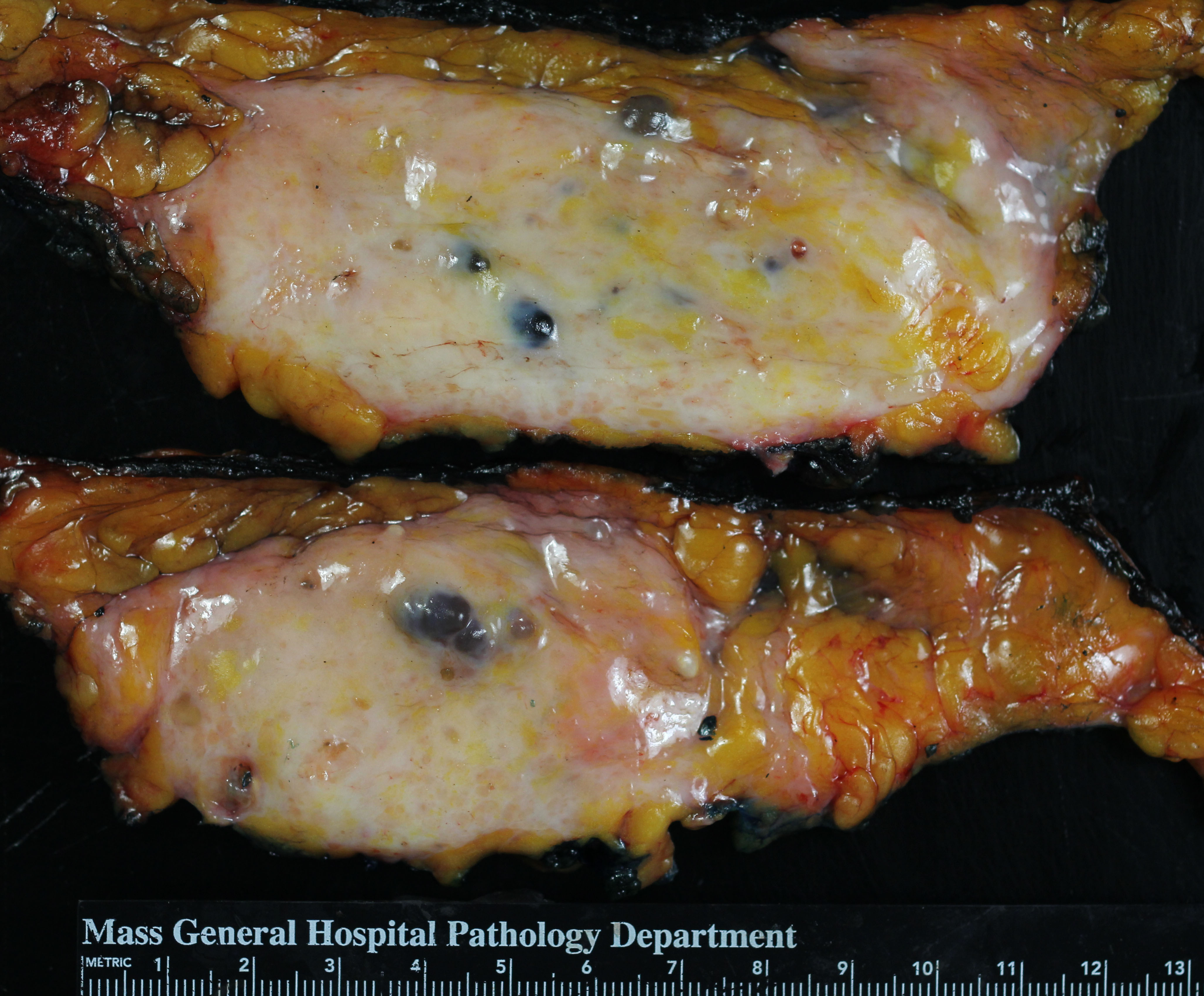
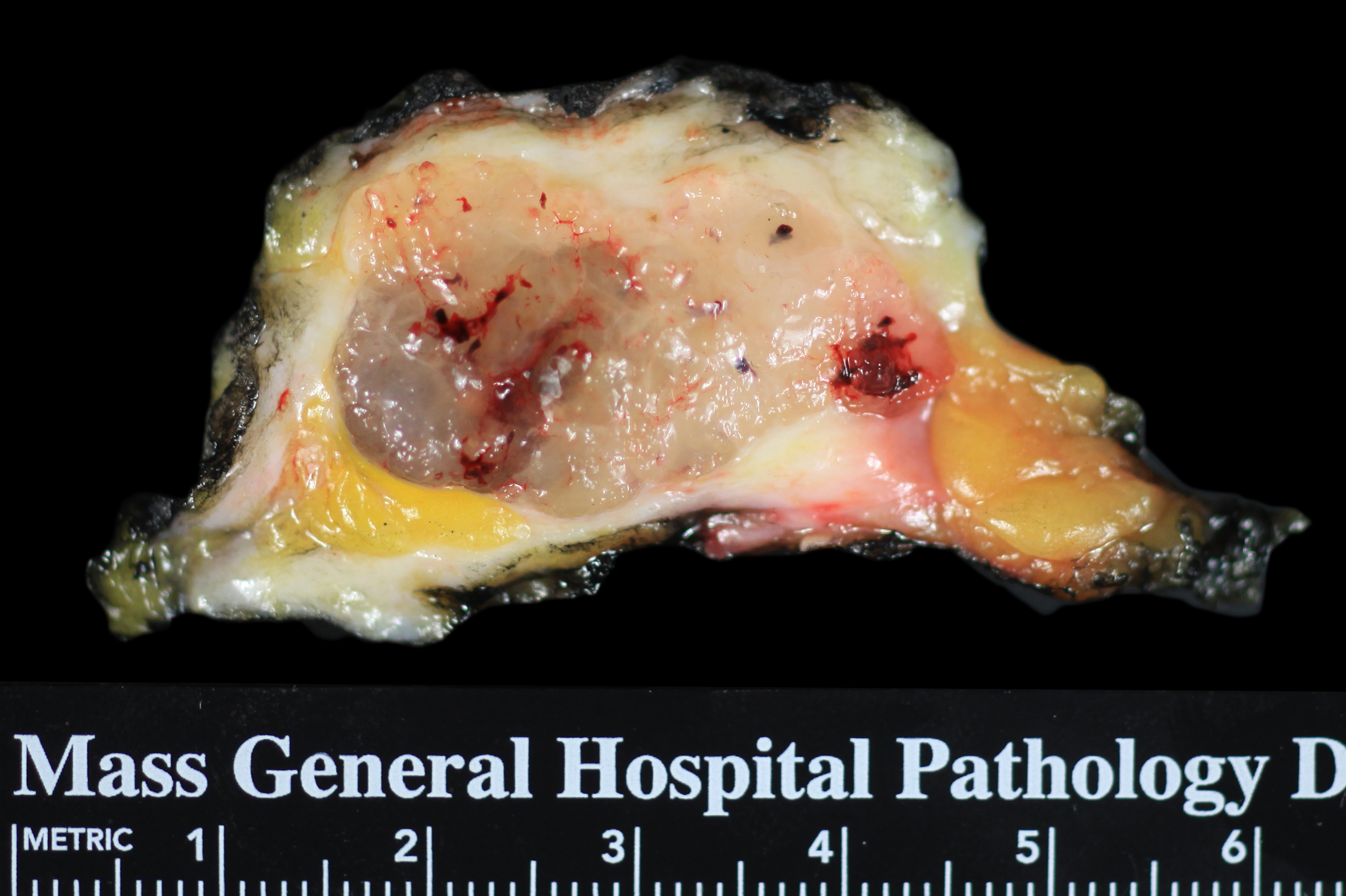
Excision alterations: The excision of tissue usually produces an easily seen abnormality a few centimeters in greatest dimension. The typical early excision site appears well defined and round or oval. Most often, it consists of a blood‑filled cavity surrounded by a rim of mottled, rubbery, yellow‑white and tan tissue; however, the features vary depending on the extent of the excision and the amount of post‑operative hemorrhage. Hemorrhage and fat necrosis represent the early changes, and depending on the size of the excision specimen, one might find a defect in the tissue. Do not confuse the relatively large vascular clips placed by surgeons with the miniscule localization clips placed by radiologists. Healing takes place over the course of several months and causes the formation of a well defined, irregular, firm, white scar.
 |
 |
Neoadjuvant chemotherapy alterations: Administration of cytotoxic chemotherapy does not alter the appearance of the pristine mammary parenchyma, but it often changes the appearance of a carcinoma (see below).
Fibrocystic Changes
Fibrocystic changes result in the formation of cysts and ill defined fibrous regions. Cysts range from a millimeter to several centimeters. Most commonly, they arise in acini, are less than 0.5 cm, and are called microcysts. When cysts reach diameters of 0.5 cm or greater, they are classified as macrocysts. Unopened cysts often look blue (they were once called blue dome cysts). Cysts have smooth linings and contain thin, pale yellow fluid. Most have a thin wall, although fibrosis and chronic inflammation surrounding macrocysts can form a distinct capsule. Spontaneous hemorrhage into a cyst does not take place often; however, when bleeding occurs, the cyst contents become turbid and blood-stained. Deposition of collagen within lobules (intralobular fibrosis) causes the formation of poorlydefined, firm, white areas, which one can appreciate more easily by touch than by sight.
 |
 |
Benign Nodules
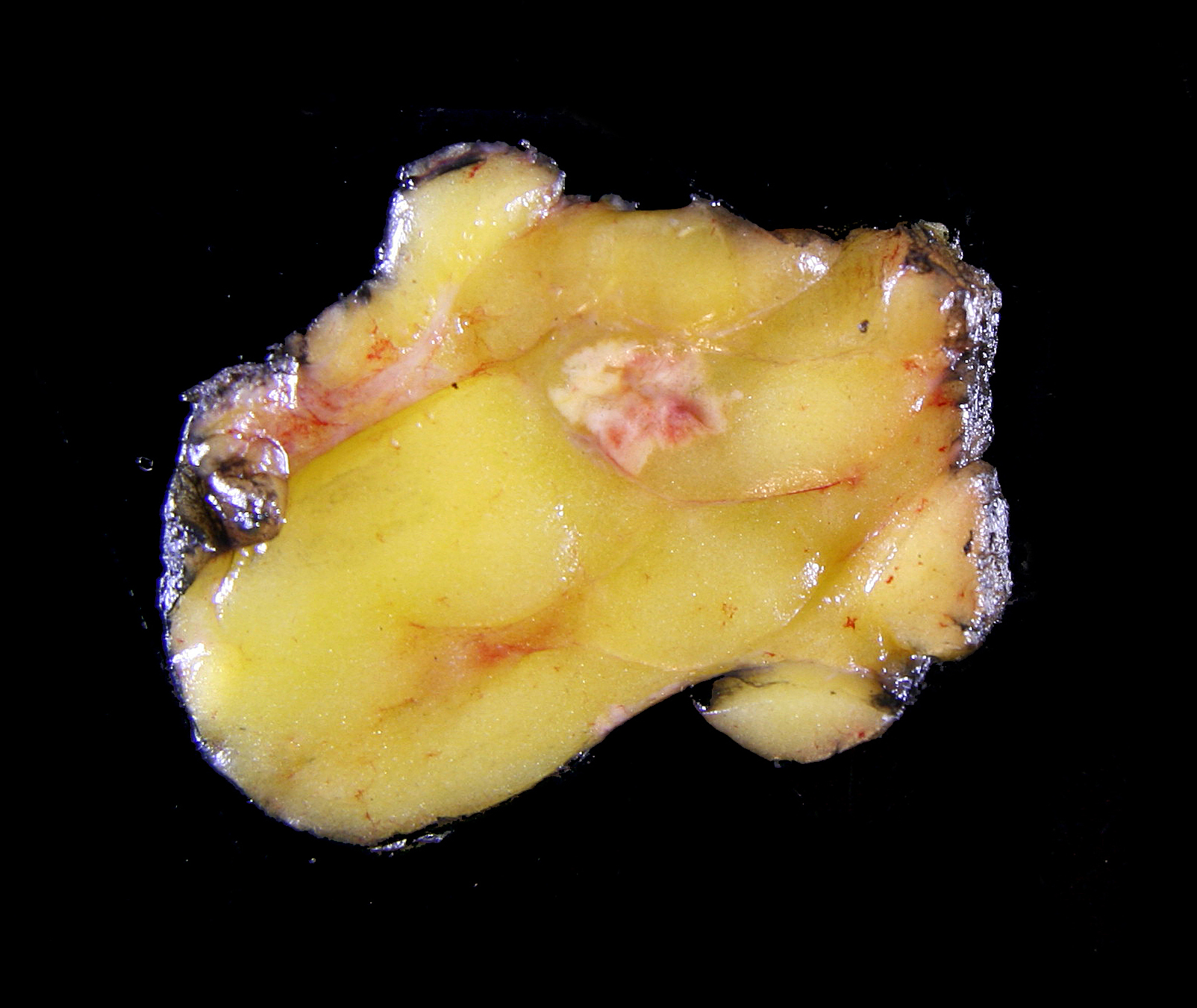
Benign neoplasms and stromal nodules appear well defined; they stand out clearly from the normal parenchyma. They have oval or round shapes and smooth borders and they usually bulge from the transected surface. The color depends on the composition of the mass. Fibrous tissue appears white, glandular tissue tan, myxoid tissue grey and glistening, and fat yellow. Hemorrhage and necrosis occur only in unusual circumstances. Most benign nodules feel rubbery; those composed of fat feel soft.
 |
 |
 |
 |
Invasive Carcinoma
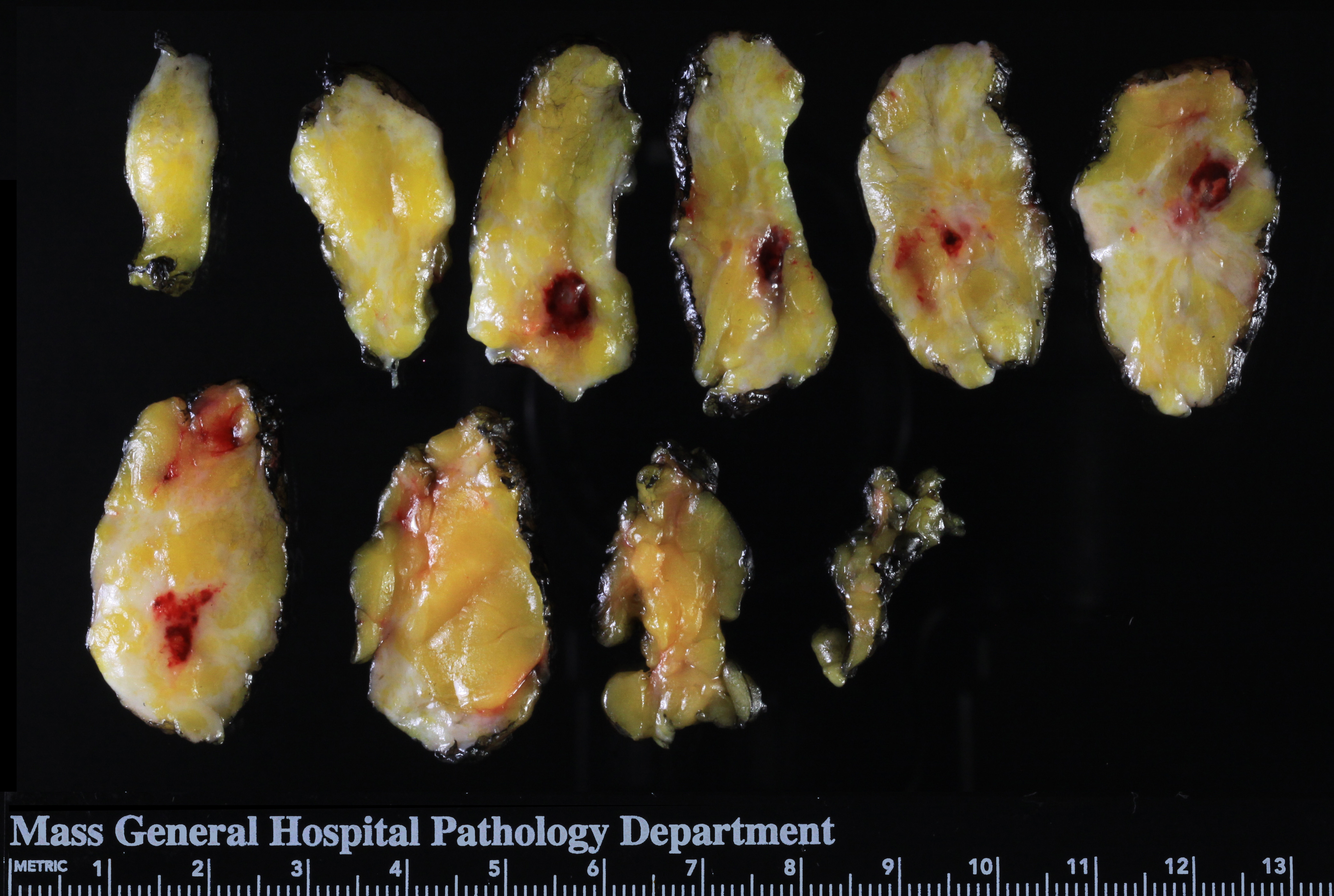
Invasive carcinomas vary widely in their features; consequently, one cannot list attributes common to all carcinomas. Most invasive carcinomas form poorly defined, irregular masses that feel firm or hard and consist of white, tan, and pale yellow tissue. The fibrotic reaction to the carcinoma cells prevents the mass from bulging from the cut surface. Focal hemorrhage usually indicates the site of a core biopsy. Microscopic extension of the carcinoma into fat causes it to take on a deep yellow color (referred to as butter yellow by Dr. Castleman). Many carcinomas deviate from these generalizations. For example, carcinomas can appear round, bulge from the transected surface, form bilobed masses, or exhibit spontaneous hemorrhage. Certain specialized types of carcinomas such as papillary carcinoma, mucinous carcinoma, and medullary carcinoma exhibit distinctive macroscopic findings, which allow one to suspect the diagnosis. Papillary carcinomas form fragile, friable, hemorrhagic masses; mucinous carcinomas form soft, glistening, grey tan nodules, and medullary carcinomas form well defined, soft, bulging, tan or grey tumors. Invasive lobular carcinomas may appear indistinct, but do not have unique macroscopic characteristics.
 |
 |
 |
 |
 |
 |
Neoadjuvant Therapy
Systemic treatment, most commonly cytotoxic chemotherapy, often alters the appearance of carcinomas. If the carcinoma disappears completely, one sees an poorly defined, irregular region of rubbery tissue with a characteristic pink grey and pale yellow hue. Pathologists refer to such a region as the tumor bed.
| Carcinoma after neoadjuvant therapy (tumor bed) | 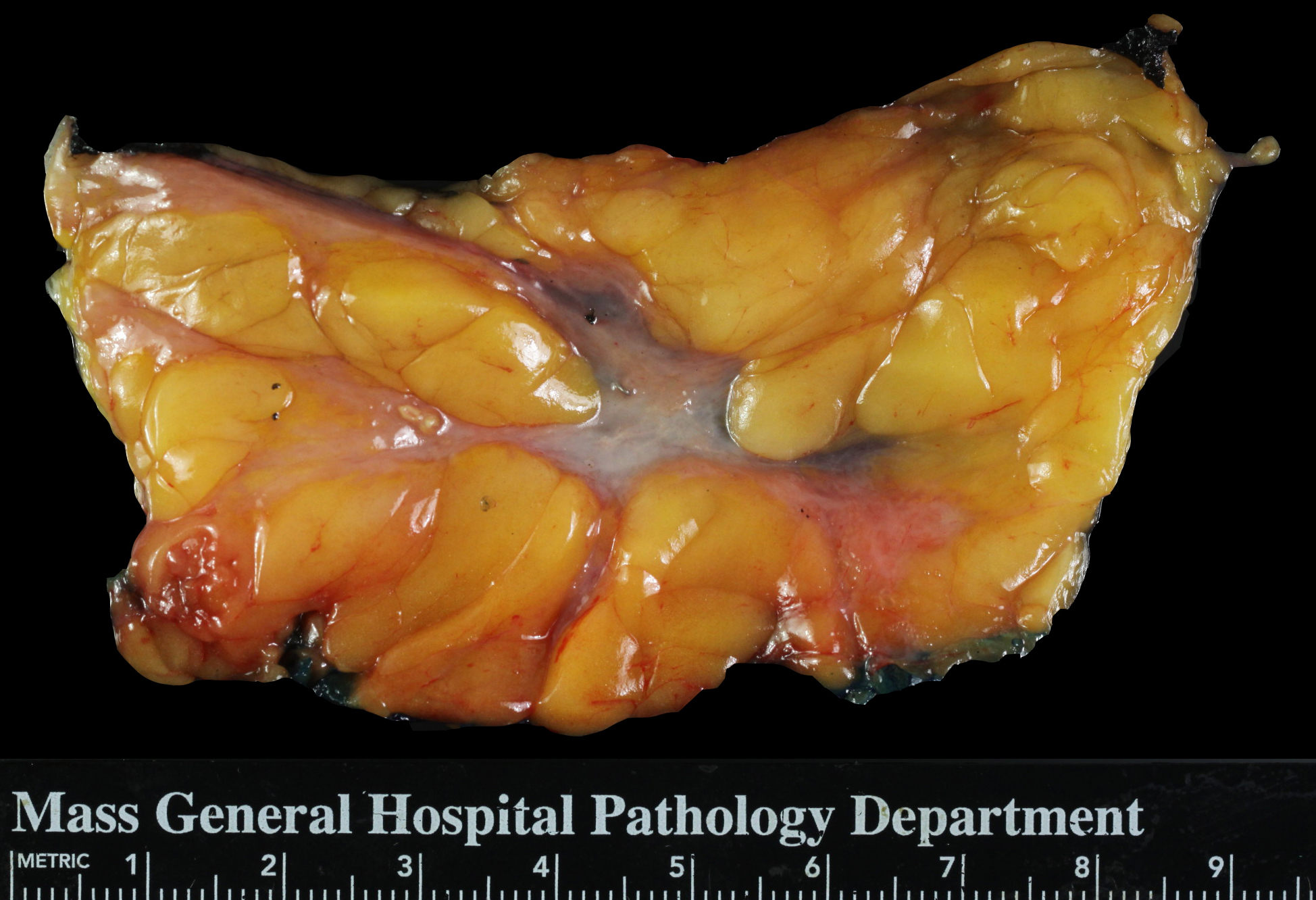 |