Difference between revisions of "mgh:cyto-1-6"
From MGH Learn Pathology
(Created page with "'''1-6 Urine Cytology: R. Tambouret MD, E. Brachtel MD, Ron Arpin SCT''' Lecture Slides: * [https://www.medialab.com/dv/dl.aspx?d=1324699&dh=bd4ef&u=111736&uh=c3cf8 Urine_Cyt...") |
|||
| (4 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
| − | + | __NOCACHE__{{DISPLAYTITLE:1-6 Urine Cytology: R. Tambouret MD, E. Brachtel MD, Ron Arpin SCT}}{{:TOC}} | |
| − | + | == Lecture Slides == | |
| − | Lecture Slides | ||
* [https://www.medialab.com/dv/dl.aspx?d=1324699&dh=bd4ef&u=111736&uh=c3cf8 Urine_Cytology--The_Big_Picture.ppt] | * [https://www.medialab.com/dv/dl.aspx?d=1324699&dh=bd4ef&u=111736&uh=c3cf8 Urine_Cytology--The_Big_Picture.ppt] | ||
<br> | <br> | ||
| Line 9: | Line 8: | ||
* Reporting and terminology | * Reporting and terminology | ||
<br> | <br> | ||
| − | + | == Basic cytomorphology == | |
Normal urothelial cells – N13-593 | Normal urothelial cells – N13-593 | ||
* Normal urothelial cells vary greatly in numbers, sizes, and shape | * Normal urothelial cells vary greatly in numbers, sizes, and shape | ||
| Line 17: | Line 16: | ||
* Round to ovoid nuclei are centrally located with finely granular chromatin and small nucleoli | * Round to ovoid nuclei are centrally located with finely granular chromatin and small nucleoli | ||
* Urothelial cells may show thin cytoplasmic tails (cercariform cells) | * Urothelial cells may show thin cytoplasmic tails (cercariform cells) | ||
| − | + | {{img4|1-6 single+transitional+cells.jpeg|1-6 umbrella+cell.jpeg|Single transitional cells: Urothelial or transitional cells have dense cytoplasm and round, central nuclei|Umbrella cells are often multinucleated}} | |
| − | Single transitional cells: Urothelial or transitional cells have dense cytoplasm and round, central nuclei | + | {{img4|1-6 nonspecific+eosinophilic+inclusion.jpeg|1-6cercariform+cells.jpeg|Non-specific eosinophilic inclusions are commonly identified in degenerating urothelial cells|Cercariform cells have an elongated cytoplasmic process with a blunted end. The cells are named for their resemblance to the cercaria developmental stage of trematodes}} |
| − | |||
| − | |||
| − | Umbrella cells are often multinucleated | ||
| − | |||
| − | |||
| − | Non-specific eosinophilic inclusions are commonly identified in degenerating urothelial cells | ||
| − | |||
| − | |||
| − | Cercariform cells have an elongated cytoplasmic process with a blunted end. The cells are named for their resemblance to the cercaria developmental stage of trematodes | ||
| − | |||
<br> | <br> | ||
'''Urothelial clusters and papillary fragments – N13-7330''' | '''Urothelial clusters and papillary fragments – N13-7330''' | ||
| Line 36: | Line 25: | ||
* Cells in the clusters show nuclei that may appear hyperchromatic or pale and may contain one or more nucleoli | * Cells in the clusters show nuclei that may appear hyperchromatic or pale and may contain one or more nucleoli | ||
* Occasionally may see a cap of umbrella cells on one side of these clusters, especially in cell groups abraded by instrumentation | * Occasionally may see a cap of umbrella cells on one side of these clusters, especially in cell groups abraded by instrumentation | ||
| − | + | {{img3|1-6 cysto+urine.jpeg|Cytoscopy often produces clusters of benign appearing urothelial cells in urine sample}} | |
| − | Cytoscopy often produces clusters of benign appearing urothelial cells in urine sample | ||
| − | |||
<br> | <br> | ||
'''Squamous and glandular cells – N13-7020''' | '''Squamous and glandular cells – N13-7020''' | ||
* Squamous cells, in variable numbers, may be present as contaminants from external genitalia or may appear as a component of normal bladder being shed from the trigone | * Squamous cells, in variable numbers, may be present as contaminants from external genitalia or may appear as a component of normal bladder being shed from the trigone | ||
* Secretory columnar cells and cells from intestinal metaplasia may be seen as part of normal metaplastic change or as a component of cystitis glandularis | * Secretory columnar cells and cells from intestinal metaplasia may be seen as part of normal metaplastic change or as a component of cystitis glandularis | ||
| − | + | {{img4|1-6 squamous_in_urine.jpeg|1-6 glandular+cells+in+urine.jpeg|Squamous cells in urine are common, especially in women from genital tract contamination|Columnar glandular cells are unusual in urine specimens; the cells probably derive from cystitis glandularis}} | |
| − | Squamous cells in urine are common, especially in women from genital tract contamination | ||
| − | |||
| − | |||
| − | Columnar glandular cells are unusual in urine specimens; the cells probably derive from cystitis glandularis | ||
| − | |||
<br> | <br> | ||
'''Renal casts – N13-7187''' | '''Renal casts – N13-7187''' | ||
| Line 54: | Line 36: | ||
* Hyaline casts are composed of amorphous, eosinophilic proteinaceous material while the granular casts are composed of degenerated red blood cells or renal tubular cells | * Hyaline casts are composed of amorphous, eosinophilic proteinaceous material while the granular casts are composed of degenerated red blood cells or renal tubular cells | ||
* Renal tubular cells are small columnar cells occurring in narrow sheets in the shape of the tubule or as single cells | * Renal tubular cells are small columnar cells occurring in narrow sheets in the shape of the tubule or as single cells | ||
| − | + | {{img3|1-6 waxy+cast.jpeg|Waxy cast: Casts take on the shape of the renal tubules in which they formed}} | |
| − | Waxy cast: Casts take on the shape of the renal tubules in which they formed | ||
| − | |||
<br> | <br> | ||
'''Ileal conduit urine – N13-7328''' | '''Ileal conduit urine – N13-7328''' | ||
| Line 65: | Line 45: | ||
* Detection of malignancy may be challenging in this setting | * Detection of malignancy may be challenging in this setting | ||
* Diagnosis should be based on cells with characteristic features of malignancy | * Diagnosis should be based on cells with characteristic features of malignancy | ||
| − | + | {{img3|1-6 ileal+loop+urine.jpeg|Loop urines usually are composed of markedly degenerated cells; the sample should be carefully examined to exclude recurrent TCC}} | |
| − | Loop urines usually are composed of markedly degenerated cells; the sample should be carefully examined to exclude recurrent TCC | ||
| − | |||
<br> | <br> | ||
'''Candida albicans – N13-7605''' | '''Candida albicans – N13-7605''' | ||
| Line 81: | Line 59: | ||
* Polyoma virus changes can be mistaken for urothelial cancer and therefore these cells are called "decoy cells"; unlike carcinoma, nuclei infected with the polyoma virus tend to be round with a smooth nuclear membrane | * Polyoma virus changes can be mistaken for urothelial cancer and therefore these cells are called "decoy cells"; unlike carcinoma, nuclei infected with the polyoma virus tend to be round with a smooth nuclear membrane | ||
* Polyoma virus may coexist with cancer | * Polyoma virus may coexist with cancer | ||
| − | + | {{img3|1-6 polyoma+virus.jpeg|Polyoma virus cytopathic effect is characterized by urothelial cells with a high nuclear to cytoplasmic ratio, a large perfectly round nucleus with homogenized chromatin}} | |
| − | Polyoma virus cytopathic effect is characterized by urothelial cells with a high nuclear to cytoplasmic ratio, a large perfectly round nucleus with homogenized chromatin | ||
| − | |||
<br> | <br> | ||
'''Catheterization/lithiasis changes – N13-5377''' | '''Catheterization/lithiasis changes – N13-5377''' | ||
| Line 90: | Line 66: | ||
* Cytologically, there is nuclear enlargement, pleomorphism, increased N/C ratio, coarse dense chromatin, prominent nucleoli, occasional mitoses, degeneration and necrosis | * Cytologically, there is nuclear enlargement, pleomorphism, increased N/C ratio, coarse dense chromatin, prominent nucleoli, occasional mitoses, degeneration and necrosis | ||
* Catheterization and instrumentation of the bladder will cause sheets and groups of urothelial cells to be sheared off; this is known as instrumentation effect and should not be confused with low grade papillary carcinoma | * Catheterization and instrumentation of the bladder will cause sheets and groups of urothelial cells to be sheared off; this is known as instrumentation effect and should not be confused with low grade papillary carcinoma | ||
| − | + | {{img4|1-6 clusters+in+bld+wash.jpeg|1-6 lubricant+in+bld+wash.jpeg|Clusters of urothelial cells may occur in urine secondary to instrumentation effect or to the presence of stones, in which case the sign out is "negative". At MGH unexplained clusters are designated as "atypical", although the likelihood of underlying low grade papillary TCC is remote|Lubricant may be present as acellular blue material in the background of an instrumented urine}} | |
| − | Clusters of urothelial cells may occur in urine secondary to instrumentation effect or to the presence of stones, in which case the sign out is "negative". At MGH unexplained clusters are designated as "atypical", although the likelihood of underlying low grade papillary TCC is remote | ||
| − | |||
| − | |||
| − | Lubricant may be present as acellular blue material in the background of an instrumented urine | ||
| − | |||
<br> | <br> | ||
'''Urothelial carcinoma – N13-7019 and N13-6041''' | '''Urothelial carcinoma – N13-7019 and N13-6041''' | ||
| Line 111: | Line 82: | ||
* Chromatin is granular and evenly distributed | * Chromatin is granular and evenly distributed | ||
* Nucleoli are indistinct or absent | * Nucleoli are indistinct or absent | ||
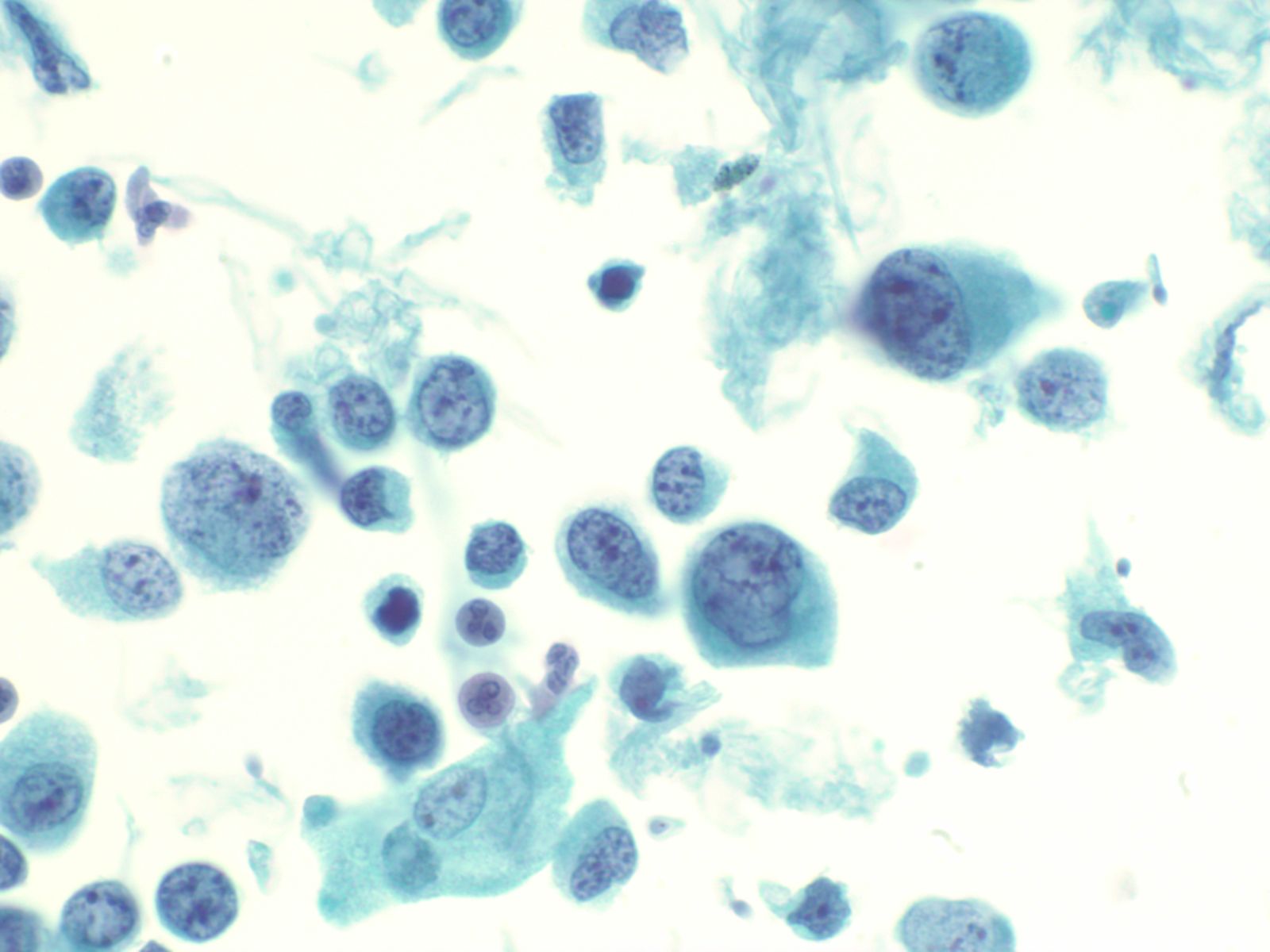
| − | + | {{img3|1-6 high+grade+TCC.jpeg|High grade transitional cell carcinoma in voided urine. The cells are variably sized with high N:C and often markedly hyperchromatic (inky) nuclei or nuclei with severe chromatin abnormalities due to aneuploidy}} | |
| − | High grade transitional cell carcinoma in voided urine. The cells are variably sized with high N:C and often markedly hyperchromatic (inky) nuclei or nuclei with severe chromatin abnormalities due to aneuploidy | ||
| − | |||
<br> | <br> | ||
'''Adenocarcinoma/squamous cell carcinoma''' | '''Adenocarcinoma/squamous cell carcinoma''' | ||
| Line 126: | Line 95: | ||
* Distant metastases may also be found in the urine, such as carcinomas, melanomas or lymphomas | * Distant metastases may also be found in the urine, such as carcinomas, melanomas or lymphomas | ||
* Tumors of the female genital tract such as squamous carcinoma and adenocarcinoma of the cervix, and high grade epithelial tumors of the ovary and colon may also be occasionally seen due to direct extension of the tumors through the bladder wall | * Tumors of the female genital tract such as squamous carcinoma and adenocarcinoma of the cervix, and high grade epithelial tumors of the ovary and colon may also be occasionally seen due to direct extension of the tumors through the bladder wall | ||
| + | {{:mgh:cytology-footer}} | ||
Latest revision as of 17:46, July 4, 2020
Contents
Lecture Slides
- Indications for cytology examination
- Procuring the specimen
- Test platforms/specimen processing and triage
- Reporting and terminology
Basic cytomorphology
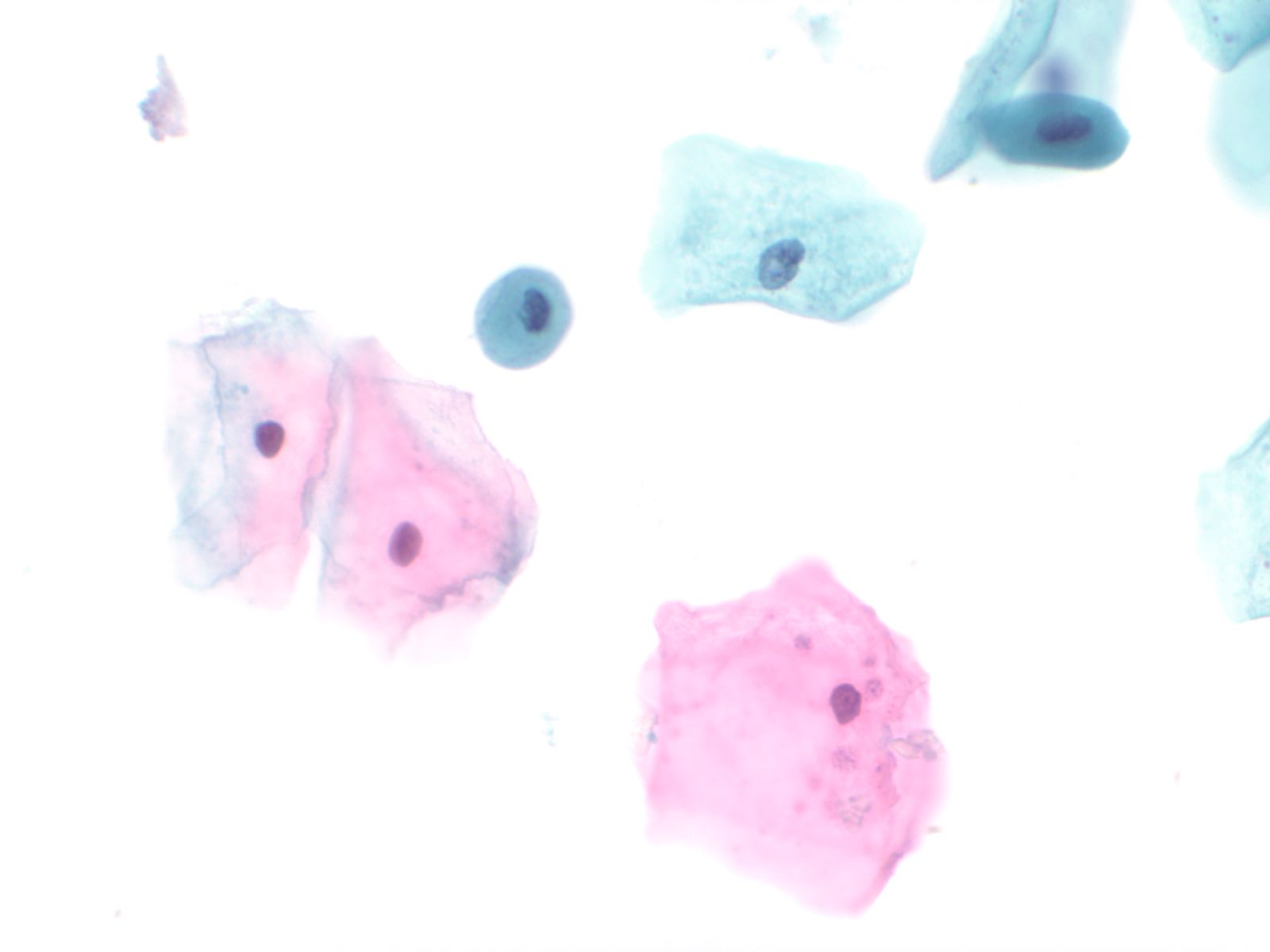
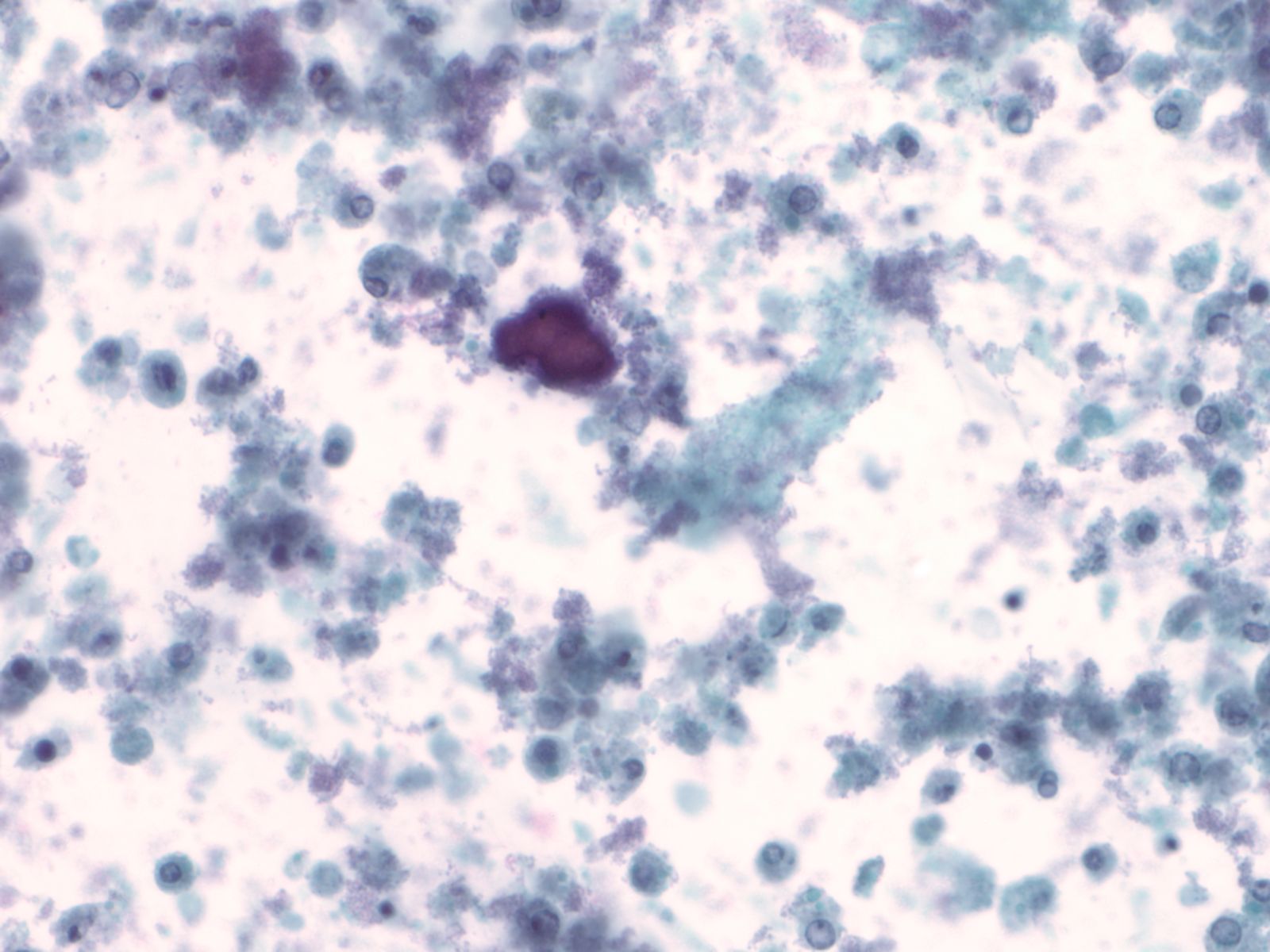
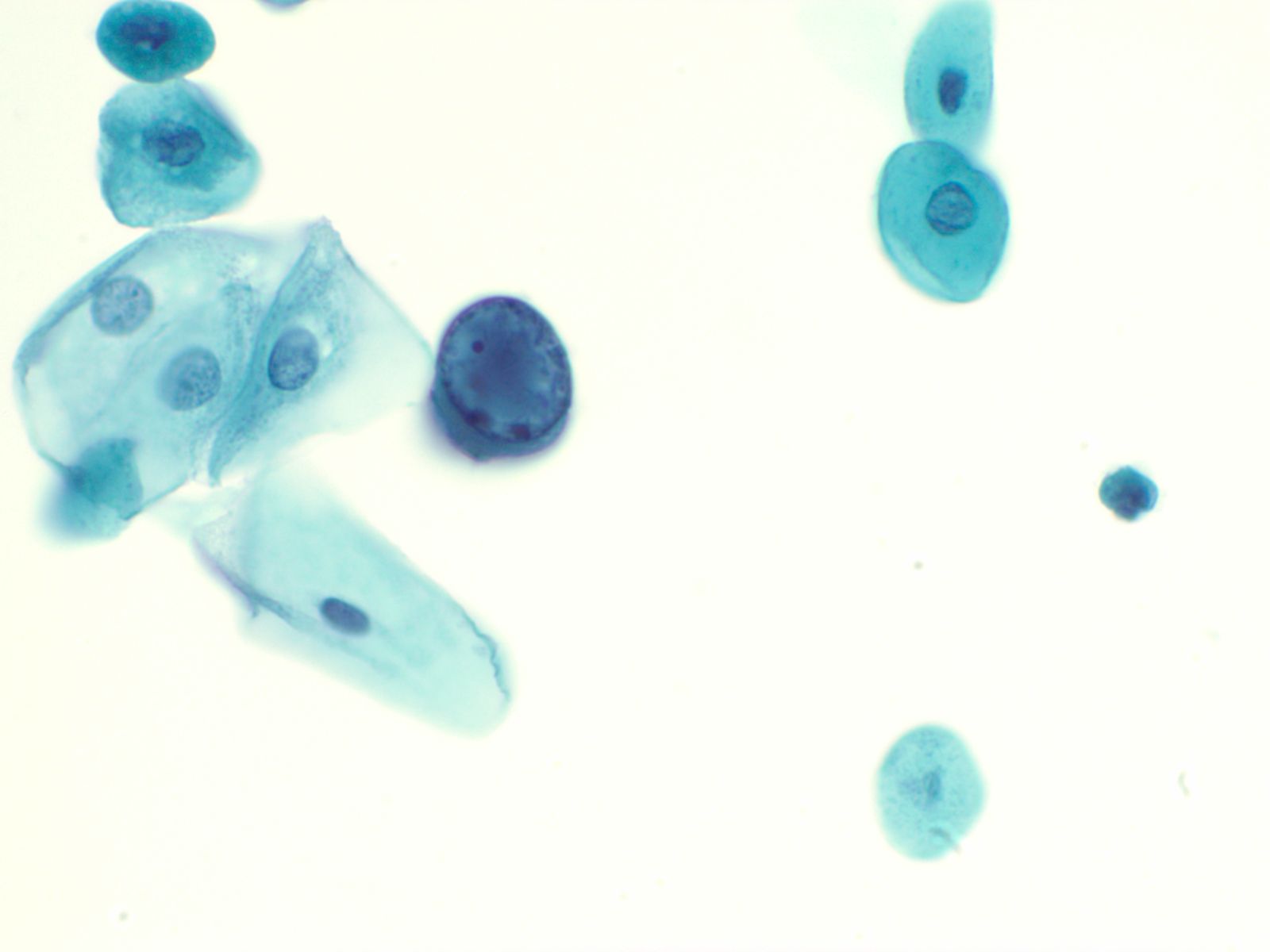
Normal urothelial cells – N13-593
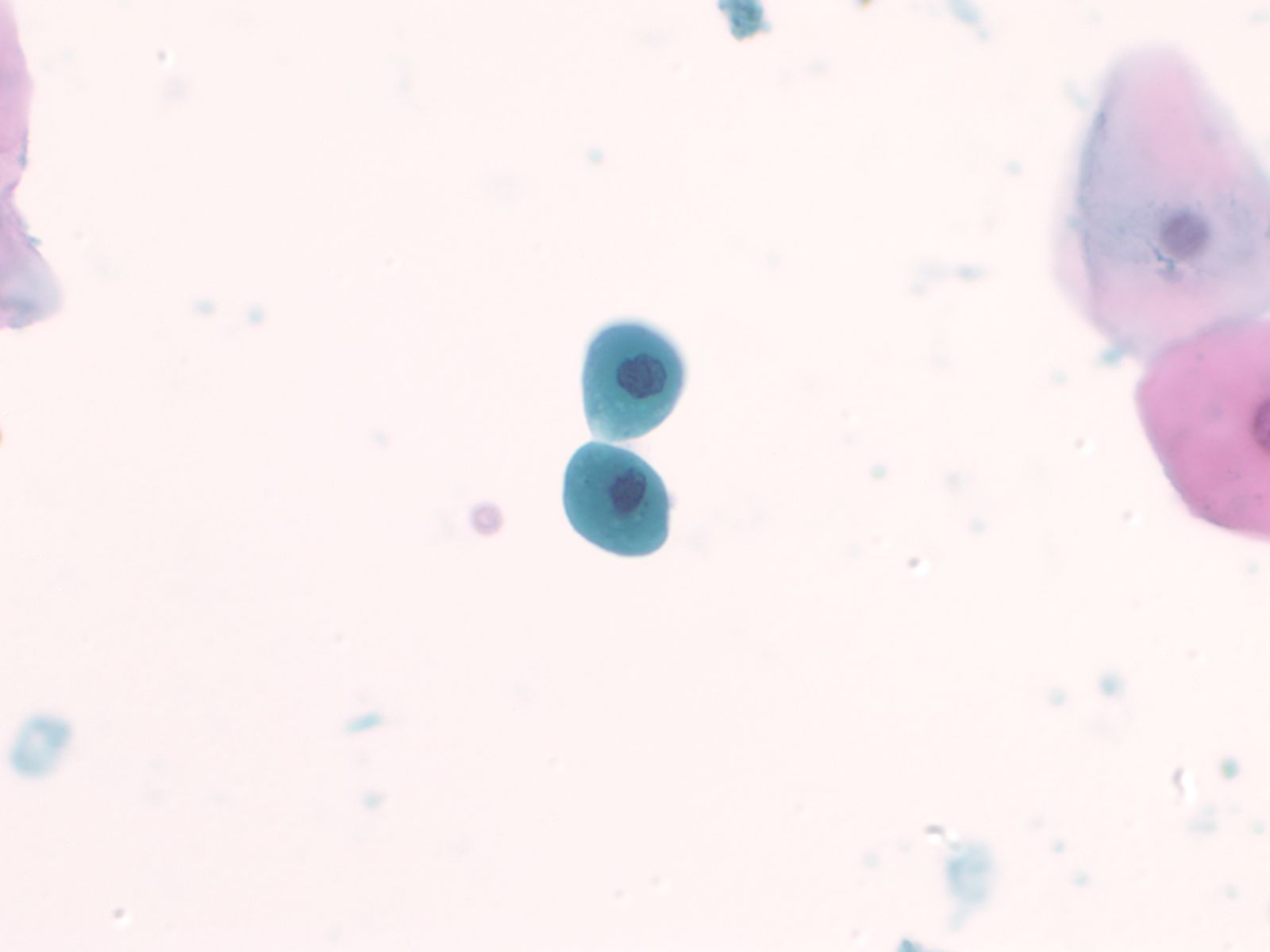
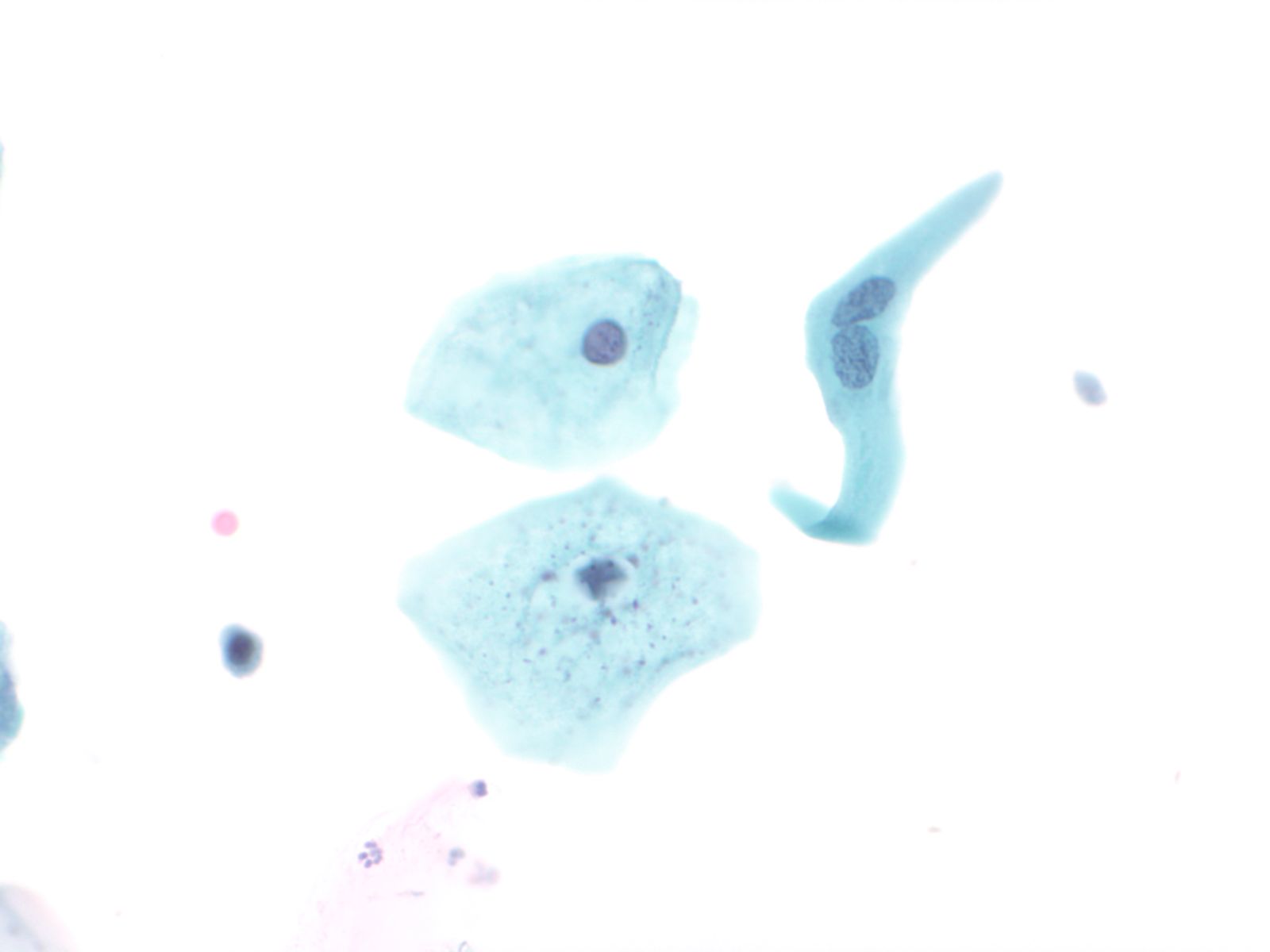
- Normal urothelial cells vary greatly in numbers, sizes, and shape
- Mononuclear urothelial cells are cuboidal, and parabasal-like or polyhedral
- Surface umbrella cells are large, often multinucleated, with convex surface corresponding to the lumen of the bladder
- Cytoplasm blue to grey and occasionally shows fine vacuolization
- Round to ovoid nuclei are centrally located with finely granular chromatin and small nucleoli
- Urothelial cells may show thin cytoplasmic tails (cercariform cells)
 |
 |
 |
 |
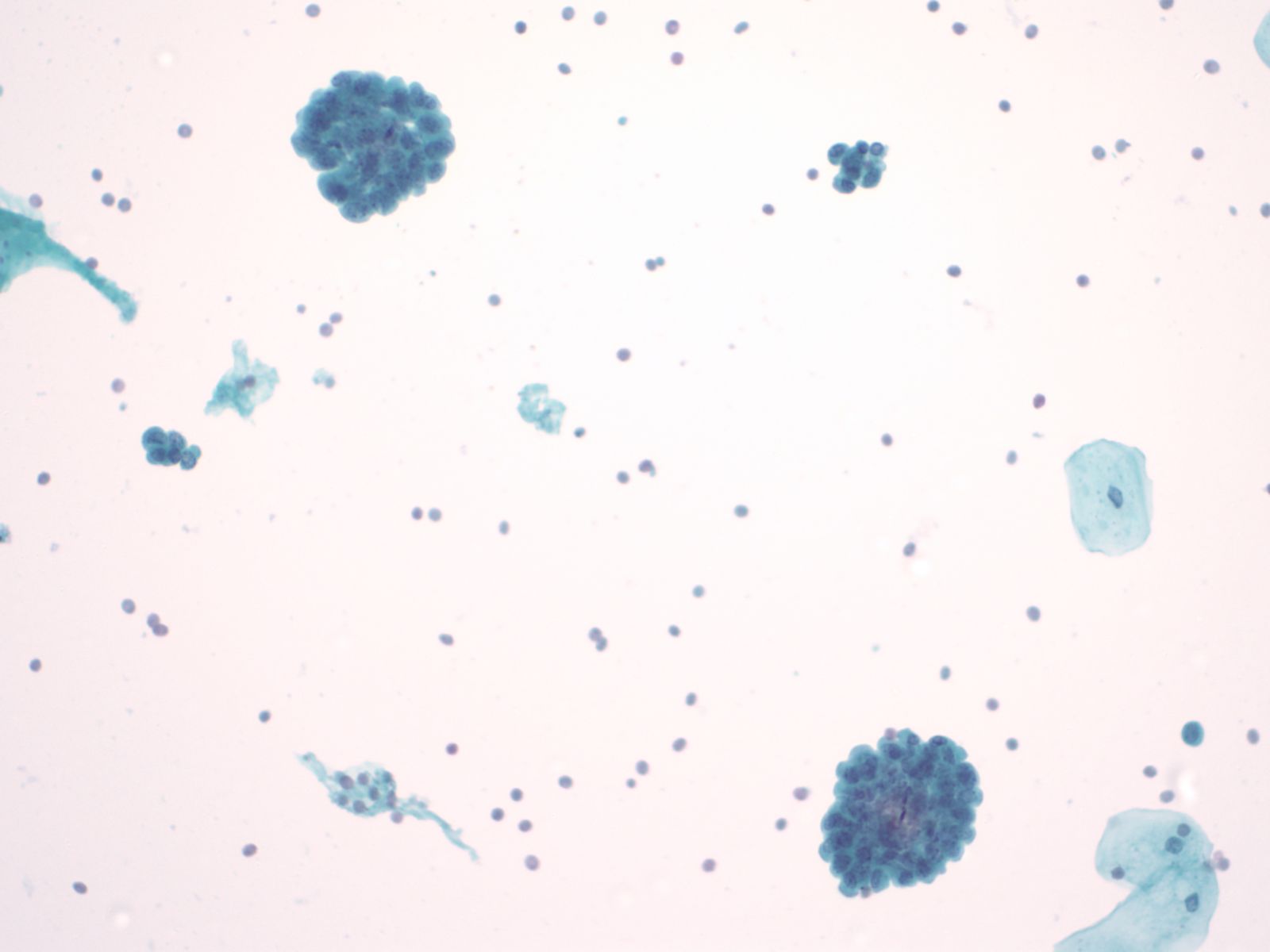
Urothelial clusters and papillary fragments – N13-7330
- Approximately 20% of normal voided urine samples may contain urothelial clusters
- This finding is considerably enhanced in bladder washings, catheterized urine, and brushings due to the propensity of urothelium to exfoliate
- The interpretation of papillary urothelial neoplasm should be made with caution and needs to be correlated with other findings
- Cells in the clusters show nuclei that may appear hyperchromatic or pale and may contain one or more nucleoli
- Occasionally may see a cap of umbrella cells on one side of these clusters, especially in cell groups abraded by instrumentation
 |
||
Squamous and glandular cells – N13-7020
- Squamous cells, in variable numbers, may be present as contaminants from external genitalia or may appear as a component of normal bladder being shed from the trigone
- Secretory columnar cells and cells from intestinal metaplasia may be seen as part of normal metaplastic change or as a component of cystitis glandularis
 |
 |
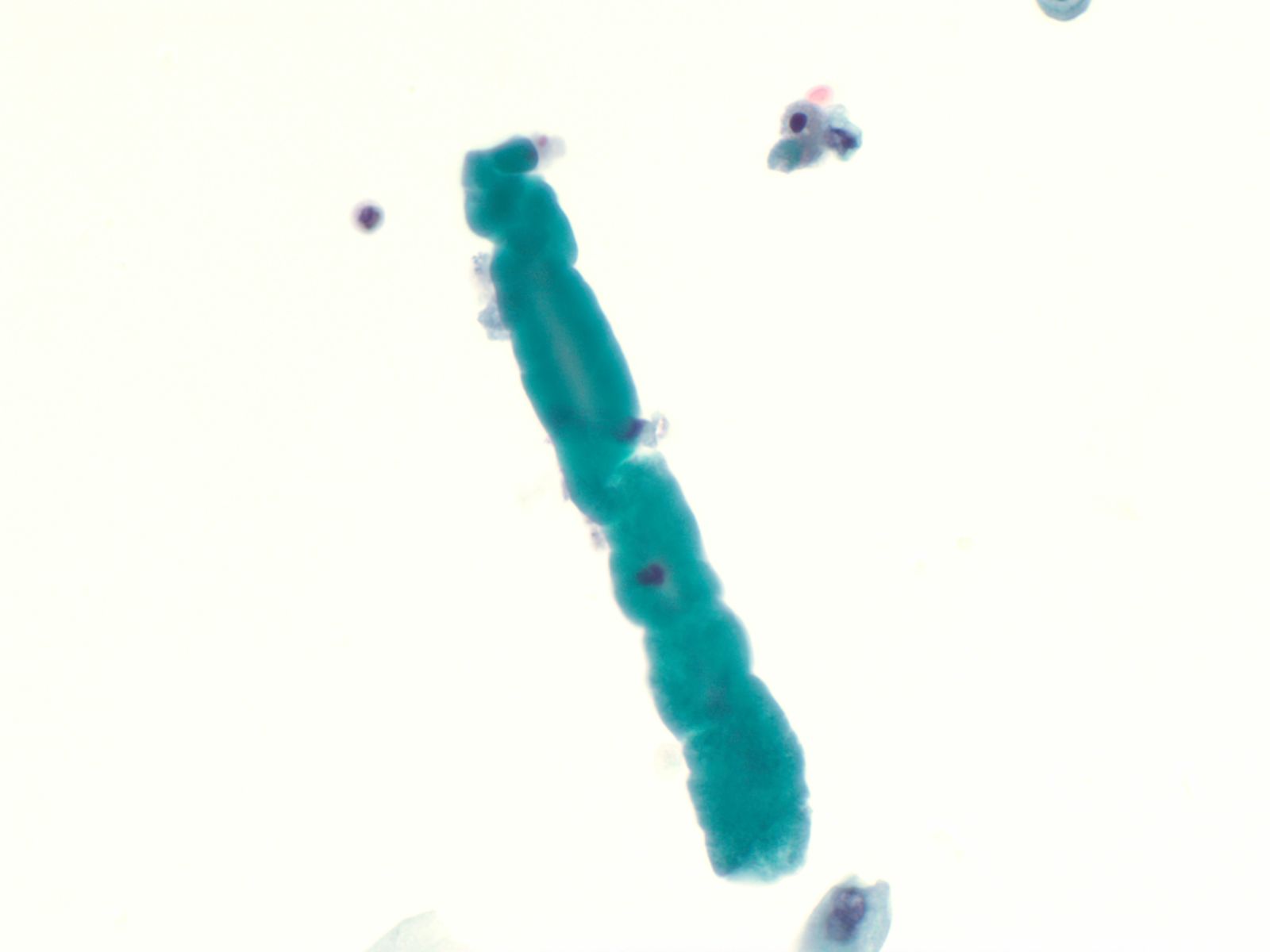
Renal casts – N13-7187
- Hyaline and granular casts may be seen even in patients without overt evidence of renal pathology
- Hyaline casts are composed of amorphous, eosinophilic proteinaceous material while the granular casts are composed of degenerated red blood cells or renal tubular cells
- Renal tubular cells are small columnar cells occurring in narrow sheets in the shape of the tubule or as single cells
 |
||
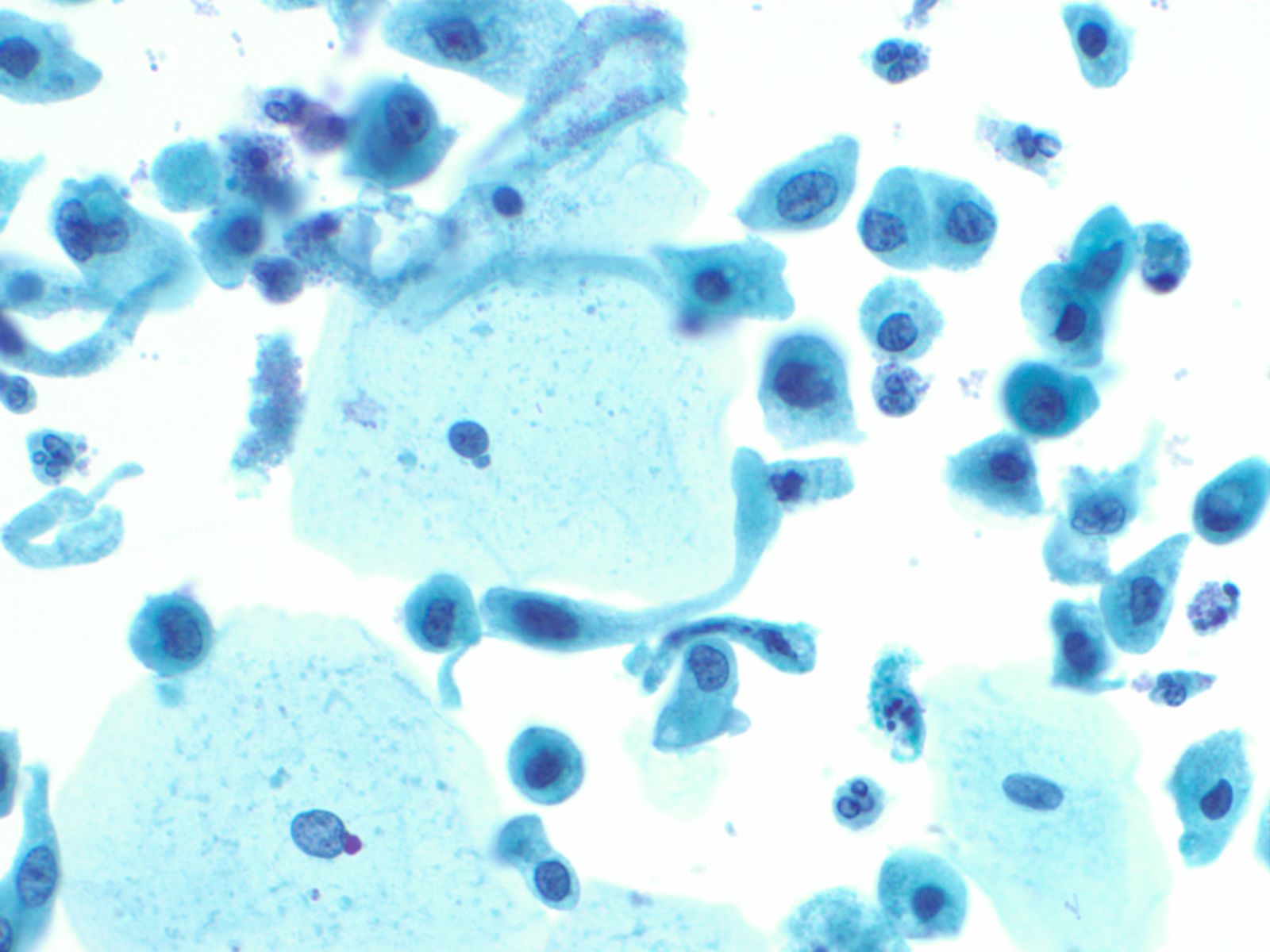
Ileal conduit urine – N13-7328
- Ileal conduit urine is usually obtained for surveillance
- Since the colonic mucosa is exposed to a hostile and toxic environment, degenerative changes predominate
- Cells resemble macrophages, there is karyorrhexis, pyknosis, and abundant red inclusions in the cytoplasm
- Cytoplasmic debris and bacteria are seen in the background
- Detection of malignancy may be challenging in this setting
- Diagnosis should be based on cells with characteristic features of malignancy
 |
||
Candida albicans – N13-7605
- Candida is the most common fungal infection and is seen as pseudo-hyphae or spores
- It may occur as a contaminant from the vagina in female patients
- However- the presence of fungal organisms in cases of renal transplant or immunosuppression denotes true infection, and requires appropriate management
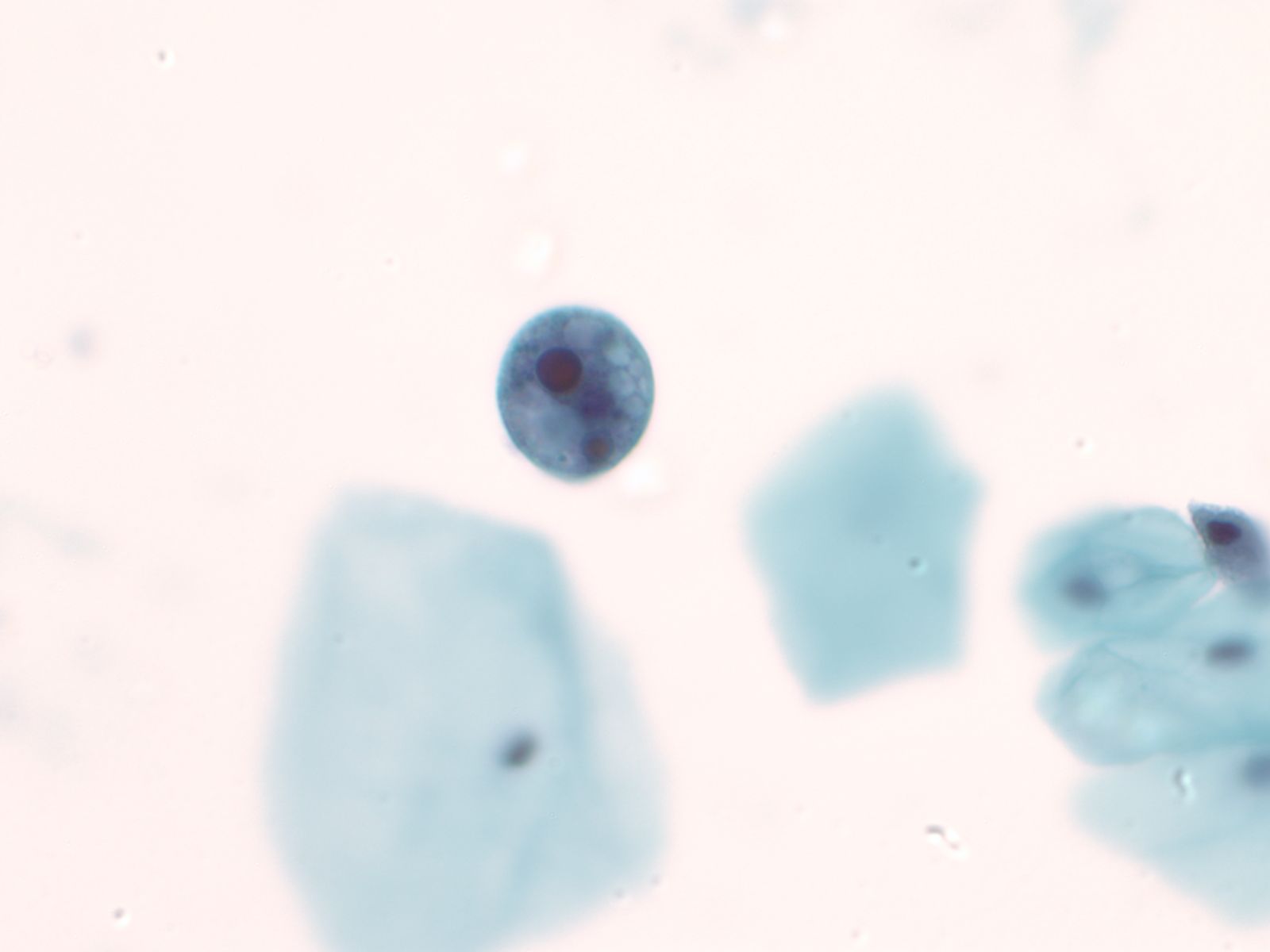
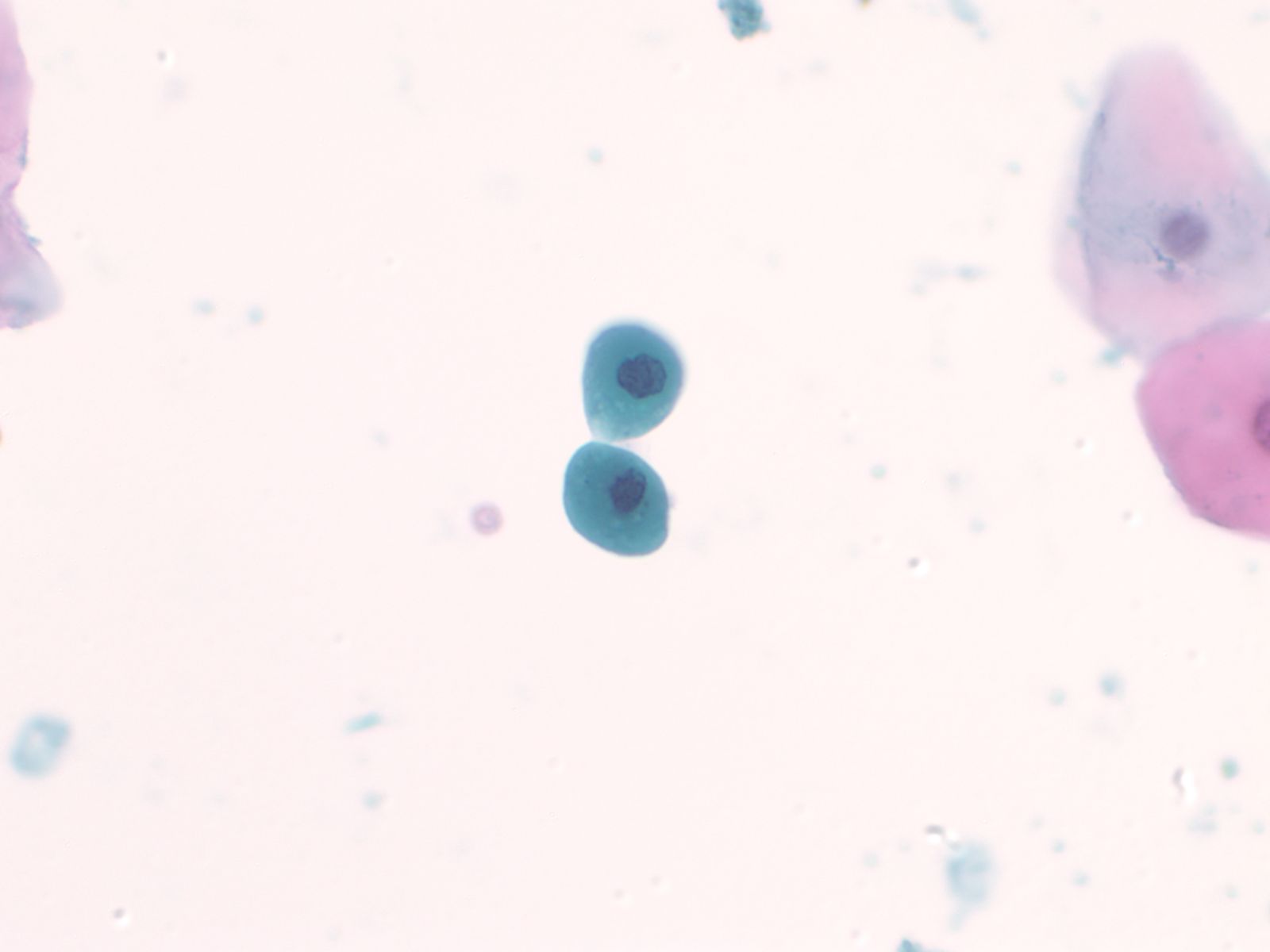
Human Polyoma Virus – N13-6375
- Infection with the polyoma virus is acquired early in life
- Activation occurs for unknown reasons or in the setting of immunosuppression due to transplantation, chemotherapy, AIDS, diabetes, etc
- Infected cells vary in size but generally have an increased nuclear to cytoplasmic ratio; viral cytopathic effect is confined to the nucleus
- Inclusions of polyoma virus are large basophilic opaque and intranuclear that fill the nucleus leaving only a thin rim of residual chromatin or net-like (reticular) filaments of chromatin
- Polyoma virus changes can be mistaken for urothelial cancer and therefore these cells are called "decoy cells"; unlike carcinoma, nuclei infected with the polyoma virus tend to be round with a smooth nuclear membrane
- Polyoma virus may coexist with cancer
 |
||
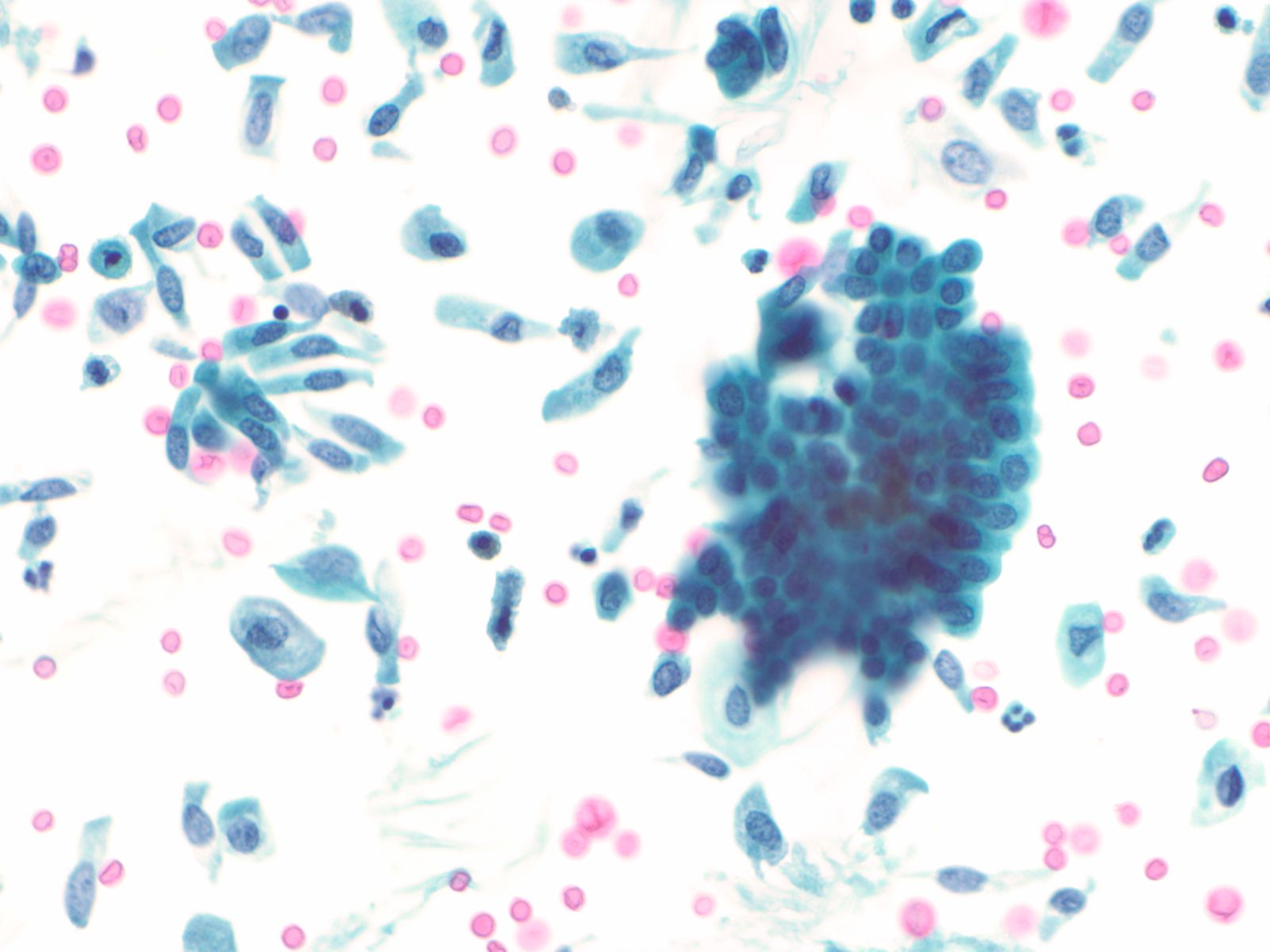
Catheterization/lithiasis changes – N13-5377
- Presence of stones can result in large urothelial clusters and papillary fragments with marked variation in the shape and size of the urothelial cells and hyperchromasia
- Sometimes the atypia associated with lithiasis is so severe that further work-up to exclude malignancy is necessary
- Cytologically, there is nuclear enlargement, pleomorphism, increased N/C ratio, coarse dense chromatin, prominent nucleoli, occasional mitoses, degeneration and necrosis
- Catheterization and instrumentation of the bladder will cause sheets and groups of urothelial cells to be sheared off; this is known as instrumentation effect and should not be confused with low grade papillary carcinoma
 |
 |
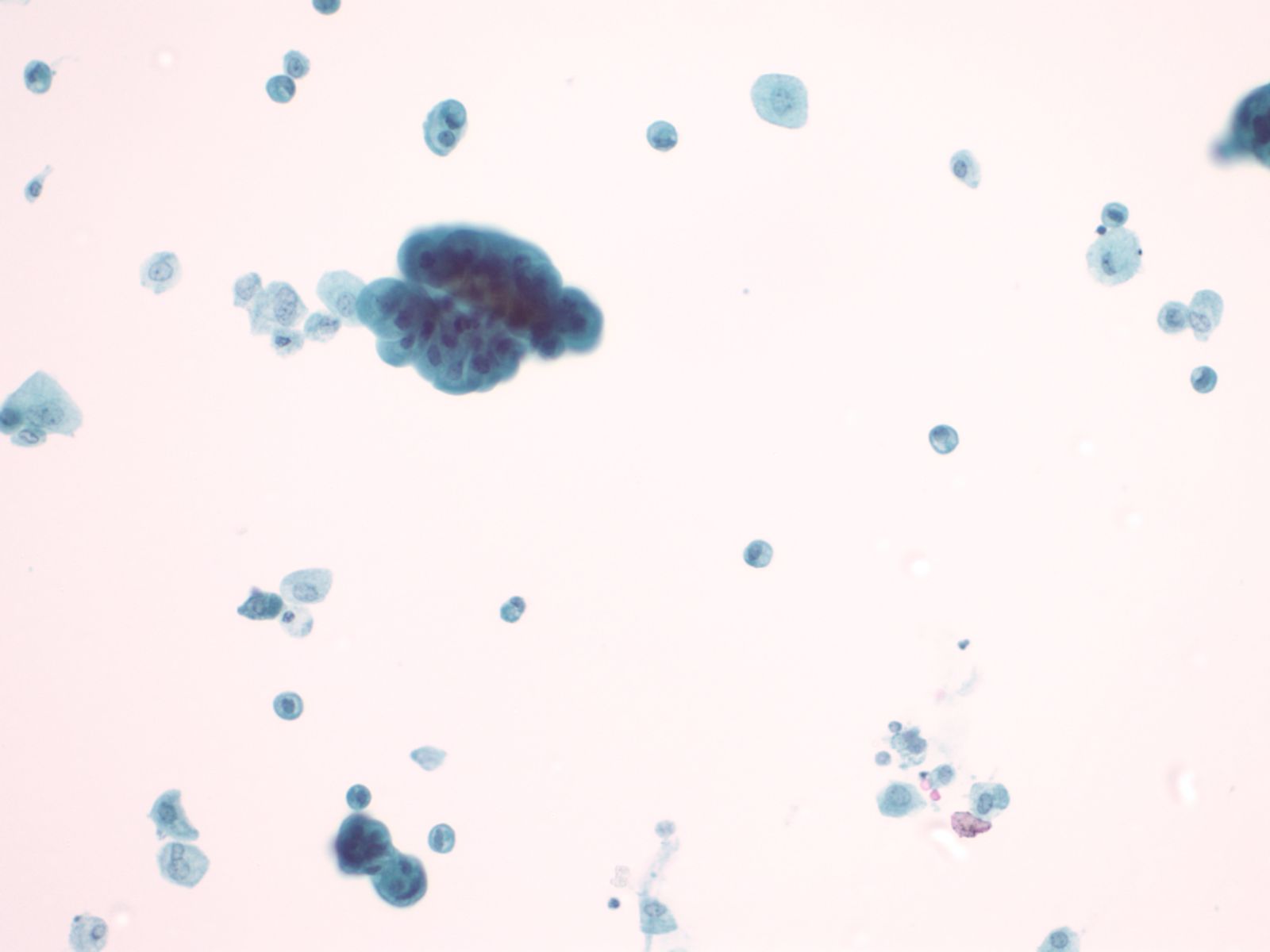
Urothelial carcinoma – N13-7019 and N13-6041
- Cytologically, high grade urothelial carcinomas are relatively easy to diagnose with a high degree of sensitivity and specificity due to the presence of anaplastic cells
- May see cellular preparations with abundant atypical urothelial clusters and single malignant cells in the background
- Occasionally the samples may be sparse
- Cells have high N/C ratios, with marked pleomorphism
- Nuclei are often eccentric with hyperchromatic coarse chromatin and large irregular nucleoli
- Nuclear membrane is thickened and occasional mitoses may be seen
- Cytoplasm is poorly demarcated and cyanophilic
- Overall, low grade urothelial carcinoma has a low diagnostic sensitivity and specificity because low grade tumors are diploid and lack the striking hyperchromasia of the high grade tumors.
- These tumors are cytologically bland, often impossible to distinguish from benign urothelial cells. three dimensional urothelial clusters in a voided urine, especially those with fibrovascular cores (a rare finding) are worrisome for low grade papillary TCC
- Cells in these clusters may have high N/C ratios with nuclei bulging out of the cytoplasm
- Nuclei may be irregular and may appear to have notches or grooves but more often than not the cells cannot be deemed worse than “atypical” , a diagnosis considered by urologists to be “negative”
- Chromatin is granular and evenly distributed
- Nucleoli are indistinct or absent
 |
||
Adenocarcinoma/squamous cell carcinoma
- Primary adenocarcinomas of the bladder are rare, constituting less than 2% of all bladder cancers
- The cells have typical features of malignancy with large eccentrically placed nuclei with open chromatin and prominent nucleoli
- Cytoplasm may be abundant and may show mucin vacuoles
- Adenocarcinoma cells may be a component of a high grade urothelial carcinoma
- Primary squamous cell carcinoma of the bladder may be secondary to Schistosomiasis infection
Metastases – N13-3279
- On rare occasions, locally invasive extravesical carcinoma may invade the bladder wall and shed into the urine, such as cells of prostatic adenocarcinoma
- Distant metastases may also be found in the urine, such as carcinomas, melanomas or lymphomas
- Tumors of the female genital tract such as squamous carcinoma and adenocarcinoma of the cervix, and high grade epithelial tumors of the ovary and colon may also be occasionally seen due to direct extension of the tumors through the bladder wall